

Background: Environmental factors including air pollutants are involved in the pathophysiology of different inflammatory rheumatic diseases (IRD) such as rheumatoid arthritis (RA) and systemic lupus erythematosus. They may influence disease activity and may trigger flares. There is currently limited data on exposure to air pollutants and its consequences on axial spondyloarthritis (axSpA). An Italian study reported the association between high concentrations of different air pollutants and poor response to bDMARDs in patients with RA, axSpA, or psoriatic arthritis (PsA) [1]. Carbone monoxide was related to the initiation of a biological agent in axSpA in another study from Taiwan [2]. The current frontier in knowledge seems to reside on i) the amplitude of the association and ii) on the critical period of exposure linked to the occurrence of a flare.
Objectives: Our study aimed to better quantify the relationships between exposure to 4 air pollutants and the occurrence of flare of axSpA and also to define the most likely critical exposure windows.
Methods: SPAir (NCT06077604) was an exploratory environmental case-cross-over study based on the data of the MISTIC cohort (a prospective clinical cohort of IRD: RA, axSpA, and PsA; NCT04191395). In this cohort, we are prospectively collecting clinical, biological and imaging data, and disease activity and treatments of the patients from the University Hospital of Besançon, France. Only patients with axSpA were considered here. We defined: 1) the case-periods corresponding to the time frame starting before a flare and 2) for each case-period, four control-periods chosen at distance of the flare and the case- period. Residential exposure to air pollutants was evaluated from the patient’s home address and using daily modeling concentrations that were established by the regional Bourgogne–Franche-Comté air quality monitoring agency (ATMO BFC) using the PREV’EST modelling Platform [3]. Four air pollutants were studied: nitrogen dioxide (NO 2 ), ozone (O 3 ), particulate matter (PM) less than 10 μm in diameter (PM 10 ) and PM less than 2.5 μm in diameter (PM 2.5 ). For each pollutant, daily mean and maximum concentrations were available on a 3 km × 3 km grid mesh over the whole study area. Flares of axSpA were defined according to BASDAI score ≥ 4/10 and/or ASDAS-CRP ≥ 2.1. We quantified the air pollution exposure using 7-day periods and calculated 4 indices for each case-period and each control-period: the mean value, the cumulated dose, the peak and the mean of the peaks. For each flare, we defined eight different case periods from the week before (week-1) to the 8 th week before the flare (week-8). For each period of exposure and each pollutant index, we iteratively used a conditional logistic regression model to estimate the odds ratios (OR) associated with an increase of 10 μg/m 3 of air pollutant concentration. The presentation of these eight OR allowed us to explore the evolution of the quantified link among the eight weeks before the occurrence of a flare, and the higher OR could then be related to the most likely critical exposure windows.
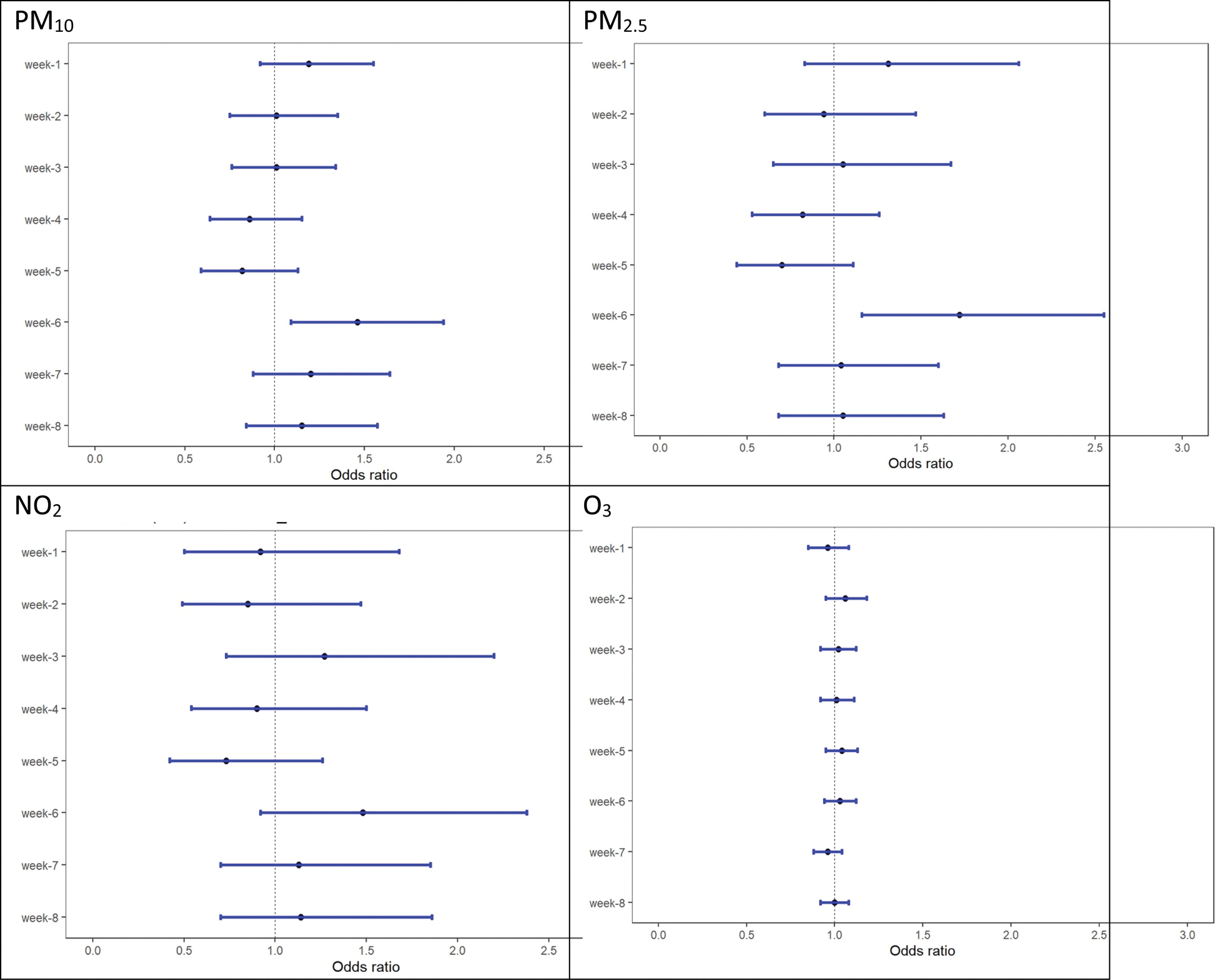
Results: Among the 378 patients with axSpA included, 242 were radiographic axSpA, 136 non radiographic axSpA; 58% were male, 77% were HLA B27+. At the date of inclusion in the MISTIC cohort, the age mean (SD) was 45 years (4 years), the mean disease duration was 11 years (11 years), a bDMARDS was present for 68%, and the mean (SD) of BASDAI and ASDAS-CRP was 4.14 (2.25) and 2.19 (1.07), respectively. Among these patients, we retained the first 182 registered flares (only one per patient) and 722 control periods between February 2020 and December 2022. The daily mean atmospheric of NO 2 , O 3 , PM 10 and PM 2.5 concentrations were 7.9, 58.2, 13.0 and 7.6 μg/m 3 , respectively. The highest OR associated with the occurrence of a flare were related to the mean value and the cumulated dose. For PM 10 , PM 2.5 and NO 2 , the highest OR were associated with the week-6 period: 1.46 (95% confidence interval (95% CI): 1.09- 1.94), 1.72 (95% CI: 1.16-2.55) and 1.48 (95% CI: 0.92-2.38) respectively. For O 3 , the highest OR were associated with the week-2 period: 1.06 (95% CI: 0.95 1.18) (Figure 1).
Conclusion: This exploratory study is the first approach focused on atmospheric exposure triggering a flare-up in patients with axSpA. We also proposed the first definition of the induction time between environmental exposure and flares. Our results are in line with a potential significant influence of atmospheric pollutants (mainly PM) on the occurrence of a flare-up in patients with axSpA. The most likely critical exposure windows could be situated one/two weeks before and six weeks before the flare. These results should be confirmed first by adjusted and stratified analysis, and if confirmed, could then provide crucial information for confirmatory studies.
REFERENCES: [1] Adami G et al, ACR Open Rheumatol. 2021.
[2] Kao CM et al. Arthritis Res Ther. 2023.
[3] Gauthier-Manuel H et al. Environ Int. 2023.
Relationships between the occurrence of a flare and the weekly mean value of air pollution for PM 10 , PM 2.5 NO 2 and O 3. Evolution of the odds ratio (OR) when considering iteratively a range of week exposure periods, from the week before (week -1) to the 8 th week before the flare (week-8). The OR were modeled using a conditional logistic regression; they were expressed for an increase of 10 μg/m 3 of air pollutant atmospheric concentration around the residential building of the subjects.
Acknowledgements: This work was supported by a grant from CHU Besancon.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (