

Background: Sociodemographic factors, such as ethnicity and socioeconomic position, have been associated with outcomes across many diseases. The majority of patients with JIA commence methotrexate as the current standard first-line disease-modifying treatment. However, to date, outcomes following treatment with methotrexate in JIA have not been investigated by ethnic group and socioeconomic position.
Objectives: This analysis aims to investigate changes in disease activity and treatment persistence following initial treatment with methotrexate in children and young people with JIA, by ethnic group and socioeconomic position.
Methods: Patients with JIA who started methotrexate between January 2004 and November 2017 and registered in the UK JIA Biologics Register at the point of starting methotrexate were included. The primary outcome was the mean change in Juvenile Arthritis Disease Activity Score (JADAS-71) between baseline and 6 months of follow-up. Multivariable linear regression was used to assess the association between ethnicity (grouped as White, Mixed, Asian and Black) or relative deprivation (using quintiles of the Index of Multiple Deprivation, IMD), and change in JADAS, adjusted for age, gender, time since diagnosis, baseline JADAS, ILAR category, and interaction between ethnicity and IMD. Treatment persistence with methotrexate (without concomitant biologic DMARDS) was analysed using Kaplan-Meier estimates. Cox-proportional hazards models were used to compare drug persistence up to 12 months following initiation between ethnic groups and IMD groups, adjusted for gender, age, time between diagnosis and commencement of methotrexate, ILAR category, and an interaction term between ethnicity and IMD. Multiple imputation was used to handle missing data.
Results: A total of 831 patients were included (Table 1). Median age 9 years, 70% female, 87% White ethnic group (3% Mixed, 8% Asian, 2% Black), 23% in most deprived quintile. Six months after starting methotrexate, mean change in JADAS for children of White ethnicity was -10.5 units (95% CI -11.5, -9.6), indicating overall improvement. Compared to those with White ethnicity, children with Black ethnicity experienced an overall lesser mean improvement in JADAS of 6.2 units (95% CI 0.9, 11.5). Children of Mixed or Asian ethnicity experienced similar improvement as those with White ethnicity. There was no significant difference observed in change in JADAS between those living in the most deprived areas compared to the rest of the cohort (1.1 units [95% CI -0.3, 2.5]). The interaction between ethnicity and IMD was not significant. Overall, 60% of patients remained on methotrexate monotherapy at one year (95% CI 59%, 62%), with a median treatment survival of 1.5 years (95% CI 1.3, 1.7 years). The proportion of patients remaining on methotrexate monotherapy at 12 months ranged from 55% of children with Black ethnicity (95% CI 43%, 66%) to 61% of those with White ethnicity (95% CI 59%, 62%). Children from the most deprived areas were more likely to stop methotrexate monotherapy over the 12-month period compared to other IMD groups (adjusted hazard ratio 1.35; 95% CI 1.03, 1.77). Both the unadjusted and adjusted hazard ratios were similar between ethnic groups.
Table 1.
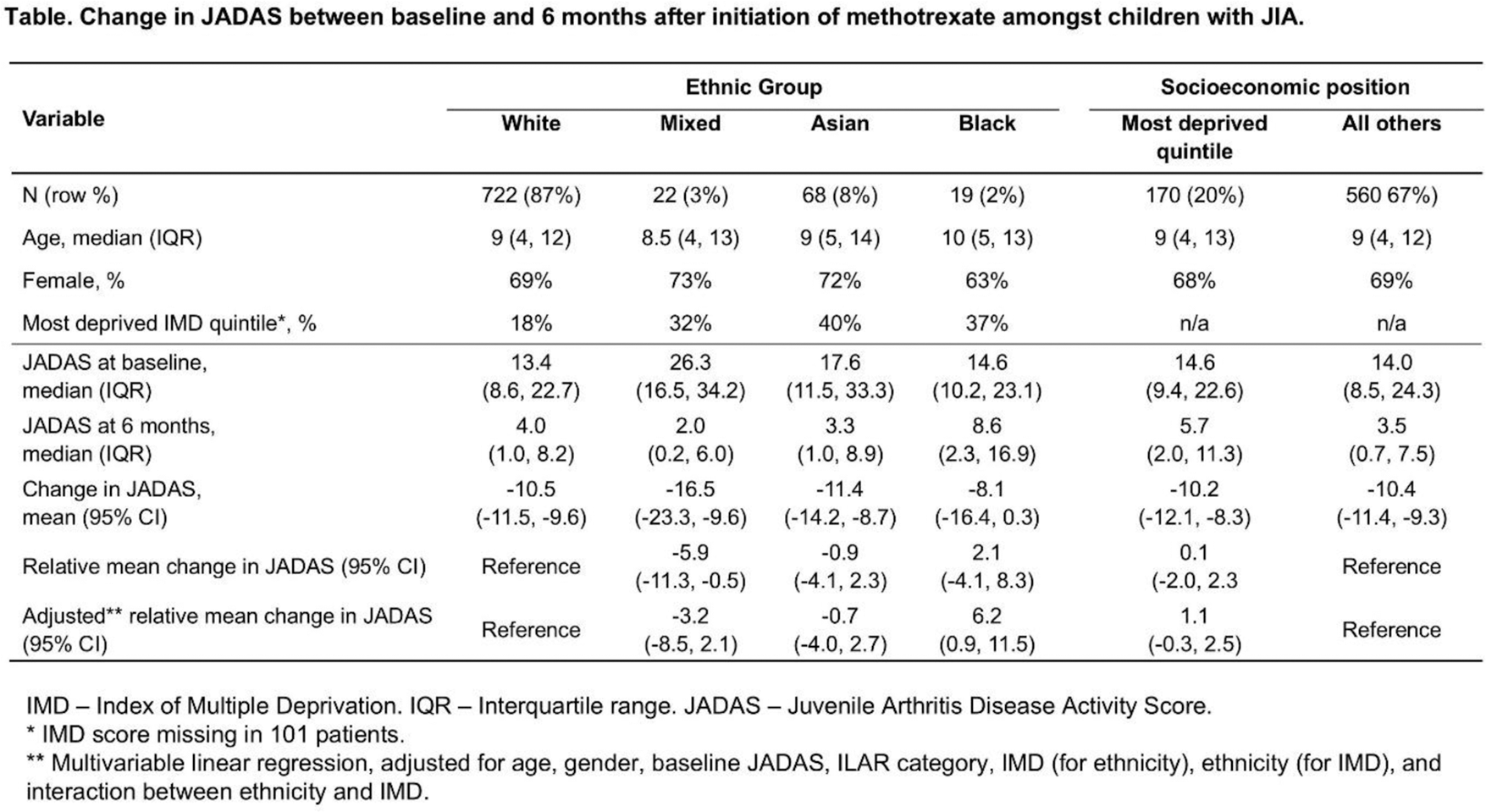
Conclusion: This analysis has shown an association between ethnicity and improvements in disease activity in the first 6 months following start of methotrexate in children and young people with JIA, independently of socioeconomic position. Children from more deprived areas were more likely to stop methotrexate during the first 12 months following initiation. Due to the small sample sizes of some of the ethnic groups, further work should be completed in larger patient groups to confirm these conclusions.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (