

Background: Digital technology has the potential to enhance rheumatology care, but its adoption in clinical workflows has been limited. Understanding clinician attitudes and preferences is crucial for effective implementation to benefit patients.
Objectives: The EULAR Digital Health and Technology Study Group was established in 2024 with the aim of building a network of multi-disciplinary experts in digital health research in rheumatic diseases. Our first objective was to develop a scoping survey among clinicians from across the multi-disciplinary team in rheumatology practice to evaluate the implementation and perceived benefits and barriers to the use of digital technologies in practice.
Methods: An English-language questionnaire, divided into four sections (demographics, implementation and barriers to use, motivators and requirements for implementation, and educational needs) was distributed online via national rheumatological societies and the Emerging EULAR Network (EMEUNET). Responses were collected and analysed using descriptive statistics.
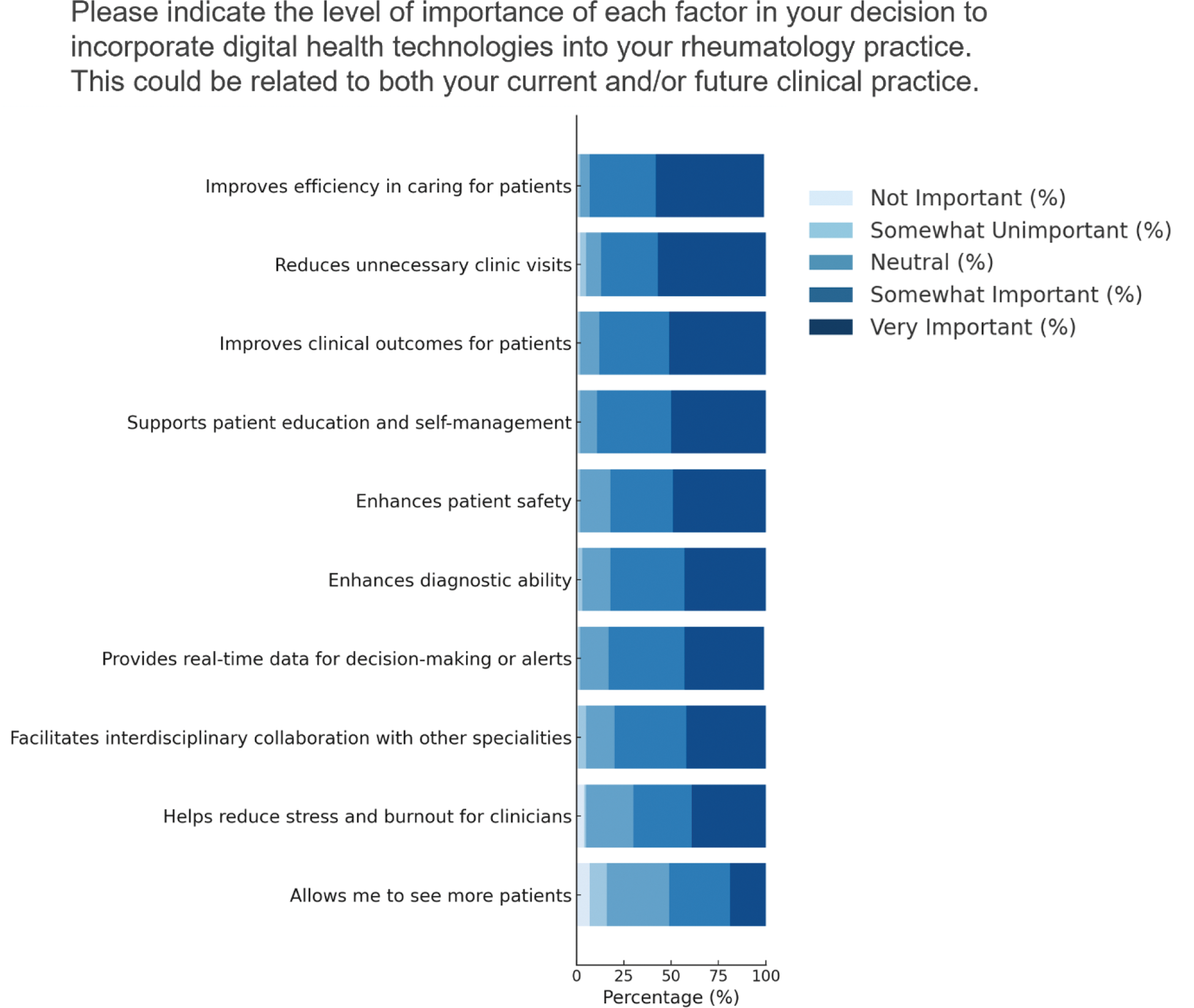
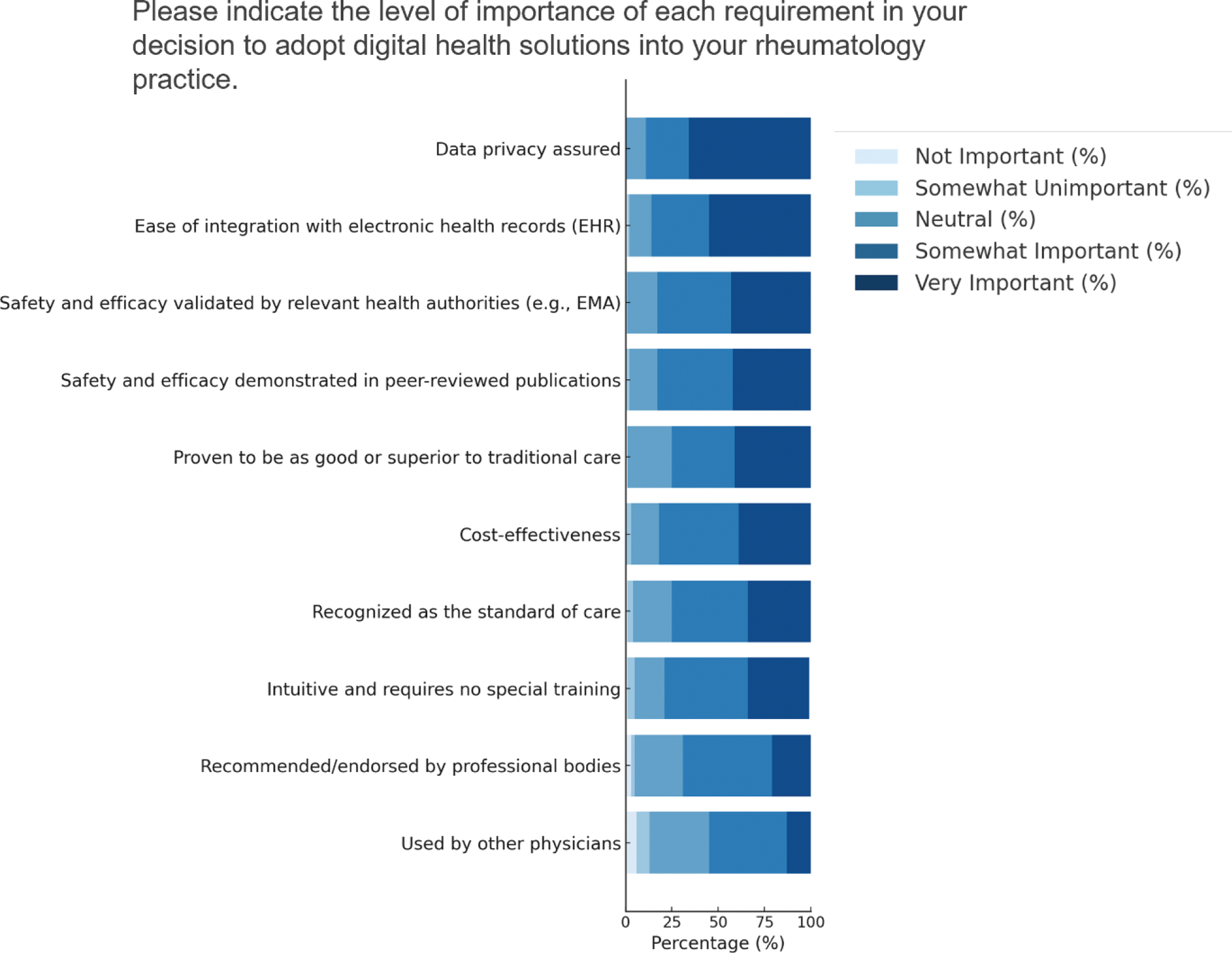
Results: A total of 136 respondents from 17 countries completed the survey. By profession, 48% were rheumatologists or trainee rheumatologists, 32% were nurses or nurse practitioners, and 20% represented other members of multi-disciplinary team including physiotherapists and psychologists. Respondents predominantly practiced in adult rheumatology (68%), with the remaining in paediatric rheumatology. Regarding implementation of digital technologies, the majority were via remote consultations which were conducted by 63.2% (86/136) of respondents. Remote patient-initiated follow-up tools including apps (24/136, 17.6%) and wearables (10/136, 7.4%) were less frequently employed. Clinical decision support systems, such as safety alerts regarding prescribing, were used by 26/136 (19.1%). The use of artificial intelligence in clinical practice was also sparsely used in contemporary practice, with 11.0% (15/136) of respondents using these technologies. The majority of which was used in automated clinical documentation (11/15, 73.3%). Only 8/136 (5.9%) of respondents reporting using software for automated image interpretation of x-rays or MRIs. Several barriers to adoption were highlighted, including integration challenges with existing systems, lack of availability of tools, cost and insufficient training. As shown in Figure 1, respondents ranked improving efficiency, reducing unnecessary clinic visits, and enhancing patient safety as the most important motivating factors for incorporating digital health technologies into their current/future practice. Supporting patient education and improving clinical outcomes were also highly valued. Regarding requirements for adopting digital technologies in practice, data privacy assurance and ease of electronic health record (EHR) integration were ranked as top priorities, followed by validated safety and efficacy (Figure 2). Cost-effectiveness and professional recommendations were moderately important, while peer adoption was rated lowest. In terms of educational needs, only 16.9% (23/136) of respondents felt very confident regarding the implementation of digital technologies in clinical practice. Most respondents expressed a preference for hands-on workshops or webinars in the areas of clinical artificial intelligence, remote monitoring and the use of mobile apps and wearables.
Conclusion: The survey reveals that, despite the potential benefits of digital technologies in rheumatology, overall adoption remains low. Clinicians prioritize tools that improve efficiency, patient safety, and education, yet face barriers such as integration challenges, lack of availability, cost, and insufficient training. Data privacy assurance and EHR interoperability emerged as critical requirements for adoption. These findings provide a helpful focus for future efforts to integrate digital tools into clinical practice. Going forward, we aim to expand this work by collecting patient perspectives to better align digital health solutions with their needs.
REFERENCES: NIL.
Key motivators for integrating digital technologies in rheumatology practice
Key requirements for integrating digital technologies in rheumatology practice
Acknowledgements: NIL.
Disclosure of Interests: Dylan McGagh Novartis, Kenneth F Baker Modern Biosciences Ltd, Clinical service improvement grant from Pfizer, Laura C. Coates AbbVie, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly and Company, Janssen, Merck Sharp & Dohme, Novartis, Pfizer, Prothena, Sun Pharma, and UCB Pharma, Max Gordon: None declared, Hanna Grasshoff: None declared, Bernd Grimm: None declared, Chloe Hinchliffe: None declared, Thomas Hügle Abbvie, Roche, Novartis, BMS, Eli Lilly, Janssen, UCB, Pfizer and Werfen, Fresenius Kabi, Abbvie, Eli Lilly and Pfizer, Heather Hunter: None declared, Norelee Kennedy: None declared, Sandrine Compeyrot-Lacassagne: None declared, Victoria Macrae: None declared, Maria Boge Lauvsnes: None declared, Polly Livermore: None declared, Jutta Richter: None declared, Silvia Del Din: None declared, Wan-Fai Ng: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (