

Background: Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by multisystem involvement and is associated with an increased prevalence of both clinical cardiovascular disease (CVD) and subclinical atherosclerosis.
Objectives: This study aimed to compare the performance of Systematic Coronary Risk Evaluation-2 (SCORE2), Framingham-REGICOR and QRESEARCH risk estimator version 3 (QRISK3) scores in identifying SLE patients at high risk of cardiovascular (CV) events, and to evaluate their predictive ability using carotid ultrasound (CU) to detect subclinical atherosclerosis.
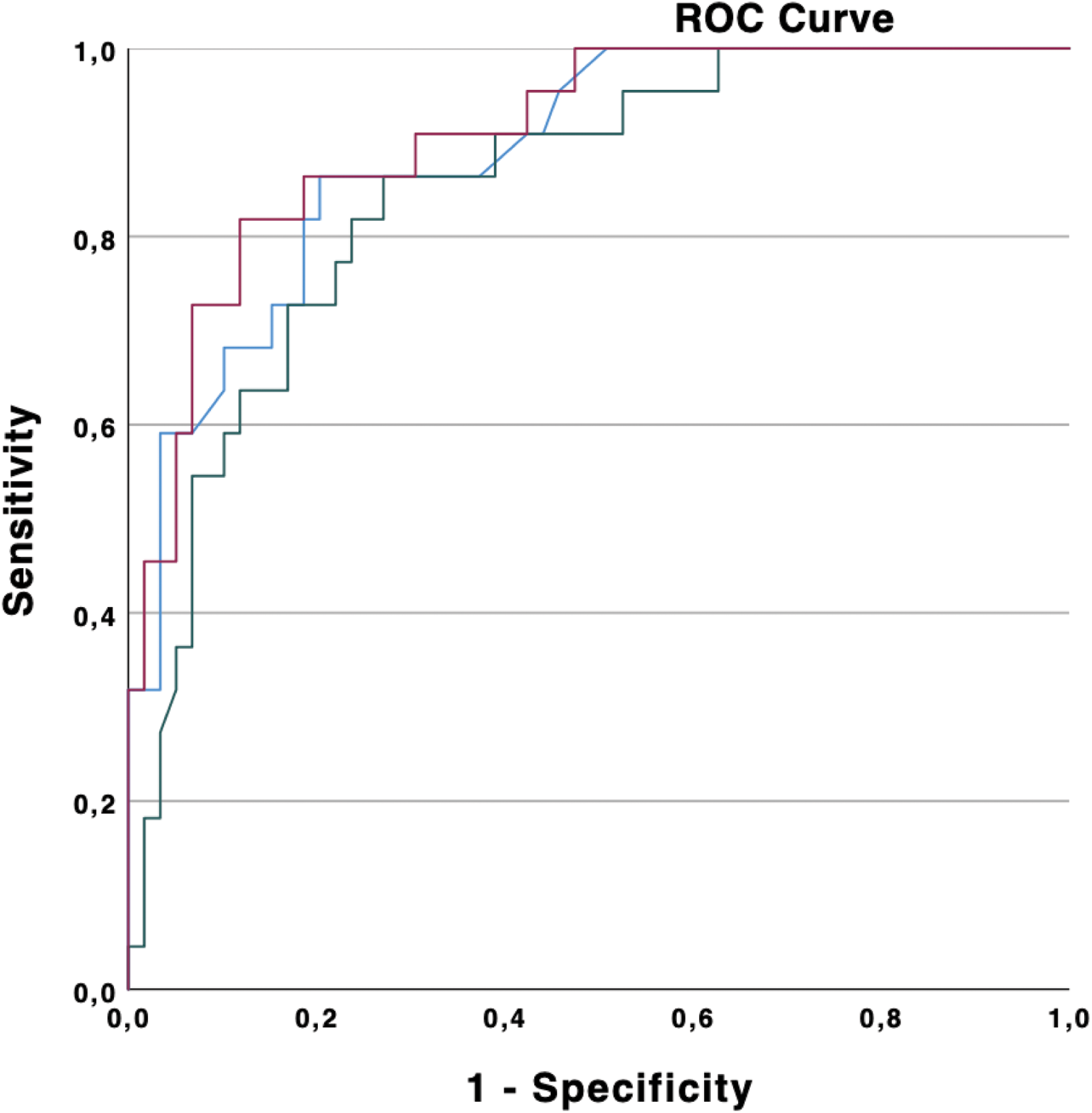
Methods: This was a cross-sectional study that included patients with SLE recruited during 2024 at the Hospital Severo Ochoa (Spain). All patients met the following inclusion criteria: 1) SLE according to the 2019 EULAR/ACR classification criteria, 2) disease duration since diagnosis ≥1 year, and 3) age between 40 and 74 years (this age range was selected based on the limitations of the CV risk scores used). Patients with a diagnosis of diabetes mellitus, chronic kidney disease, or a history of CV events were excluded from the study, as they were directly classified into a high/very high CV risk category. Surveys in patients with SLE were performed to assess CV risk factors and medication. Laboratory data related to SLE activity were also collected. Three CV risk scores (SCORE2, Framingham-REGICOR, and QRISK3) were used to estimate the 10-year risk of developing a CVD. CV risk was classified as low, moderate, high, or very high according to the percentages established by each algorithm. CU was performed to determine carotid intima-media thickness (cIMT) and detect the presence of atherosclerotic plaques.Statistical analysis: continuous variables were expressed as mean and standard deviation (SD) or as a median and interquartile range (IQR) for non-normally distributed variables. The relationship between the different CV risk scores and the results of CU (positive if IMT ≥ 0.9 mm or plaque present) was analyzed using receiver operating characteristic (ROC) curves. Area under the receiver operating characteristic curve (AUC) analyses were used to assess their predictive accuracy. A p-value of <0.05 was considered statistically significant.
Results: A total of 81 patients were included in the study. Among them, 74 (91.4%) were women, with a mean age of 53.3 (SD ± 10.1) years and a mean disease duration of 17.1 (SD ± 9.2) years. Traditional CV risk factors and pharmacological treatment are detailed in Table 1. Laboratory data showed a median C-reactive protein (CRP) level of 2 mg/dL (IQR 2) and proteinuria was identified in only 3 patients. Anti-DNA positivity was observed in 14.8% of the patients, while complement consumption (defined as decreased levels of C3 and/or C4) was present in 21% of the cohort. Disease activity, evaluated using the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K), demonstrated a median score of 1 (IQR 2), with the majority of patients classified as low disease activity. Upon applying the three CV risk scores, the following classifications were observed:
The SCORE2 tool classified 67 patients (82.7%) as low risk, 13 (16%) as high risk, and 1 patient (1.3%) as very high risk.
The Framingham-REGICOR score classified 77 patients (93.8%) as low risk, 4 (4.9%) as moderate risk, and 1 (1.3%) as high risk, with no patients categorized as very high risk.
The QRISK3 score classified 56 patients (69.1%) as low/moderate risk and 25 (30.9%) as high/very high risk.
CU was positive in 22 patients (27.16%). A cIMT ≥ 0.9 mm was identified in 21 of them, and an atherosclerotic plaque was present in 10 patients. The mean cIMT was 0.7 (SD ± 0.2) mm. CU led to the reclassification of some patients initially designated as low/moderate CV risk by the three scores studied. These patients were reclassified as high or very high CV risk in 11.1% of those evaluated by SCORE2, 24.7% by Framingham-REGICOR, and 4.9% by QRISK3. Comparing the three CV risk scores in relation to carotid ultrasound, the AUC for QRISK3 was 0.908 (95% CI: 0.839–0.976), compared to 0.889 (95% CI: 0.813–0.964) for SCORE2 and 0.849 (95% CI: 0.760–0.938) for Framingham-REGICOR, with no statistically significant difference (Figure 1).
Cardiovascular risk factors and pharmacological treatment in the 81 patients with SLE studied.
| Smoker | n*=14 (17,3%**) | |
| Body Mass Index >25 | n=42 (51,9%) | |
| High waist circumference | n=41 (50,6%) | |
| Cardiovascular risk factors | Hypertension | n=26 (32,1%) |
| Dyslipidemia | n=8 (9,9%) | |
| Antiphospholipid syndrome | n=23 (28,4%) | |
| Sedentarism
| n=64 (79,0%) | |
| Acetylsalicylic acid | n*=21 (25,9%**) | |
| Corticosteroids | n=26 (32,1%) | |
| Pharmacological treatment | Hydroxychloroquine | n=59 (72,8%) |
| Other treatments (methotrexate, azathioprine, mycophenolate mofetil, rituximab, belimumab, or anifrolumab)
| n=32 (39,5%)
|
* n = number of patients. ** % = percentage of patients.
Relationship between cardiovascular risk scores (SCORE2, Framingham-REGICOR and QRISK3) and positive results of carotid ultrasound (cIMT ≥ 0.9 mm or atherosclerotic plaque).
Conclusion: CU in SLE patients allows for early detection of subclinical atherosclerosis before the development of CVD. The results of this study show that increased cIMT and/or the presence of carotid plaque can lead to the reclassification of patients with SLE initially assessed as low/moderate CV risk by traditional scores to high or very high CV risk after ultrasound evaluation. When comparing the three CV risk scores, the findings indicate that they are equally reliable predictors of subclinical atherosclerosis. However, further studies are required to confirm these findings.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (