

Background: Inflammatory joint diseases (IJD), including rheumatoid arthritis (RA), axial spondyloarthritis (axSpA) and psoriatic arthritis (PsA), are associated with an increased risk of cardiovascular (CV) disease. A prevailing assumption suggests that RA patients experience worse outcomes after myocardial infarctions (MI) due to atypical presentations, greater myocardial damage, higher rates of in-hospital complications and less effective treatment. However, evidence supporting this assumption is limited, and data for axSpA and PsA are largely lacking.
Objectives: Our aim was to provide a clearer understanding of whether IJD patients face different clinical presentations, cardiac involvement, treatment approaches and outcomes following an initial MI compared to those without IJD.
Methods: We utilized data from the comprehensive nationwide Norwegian Cardio-Rheuma Register, which includes data from the adult Norwegian population. This registry integrates data from multiple mandatory Norwegian health registries. Diagnostic and procedure codes, including ICD-10 and NCMP codes, were used to identify RA, axSpA and PsA cases using a previously validated method. MI event data were sourced from the Norwegian Myocardial Infarction Register (NORMI), which has an almost complete capture rate of MI events in Norway and includes detailed clinical information. We excluded patients with pre-existing atherosclerotic CV disease, focusing on those experiencing their first MI to ensure relevant comparisons. Analyses were stratified by sex and adjusted for age using inverse probability (IP) weights. Dichotomous variables were analyzed using logistic regression, while continuous variables were compared using generalized linear models (GLM).
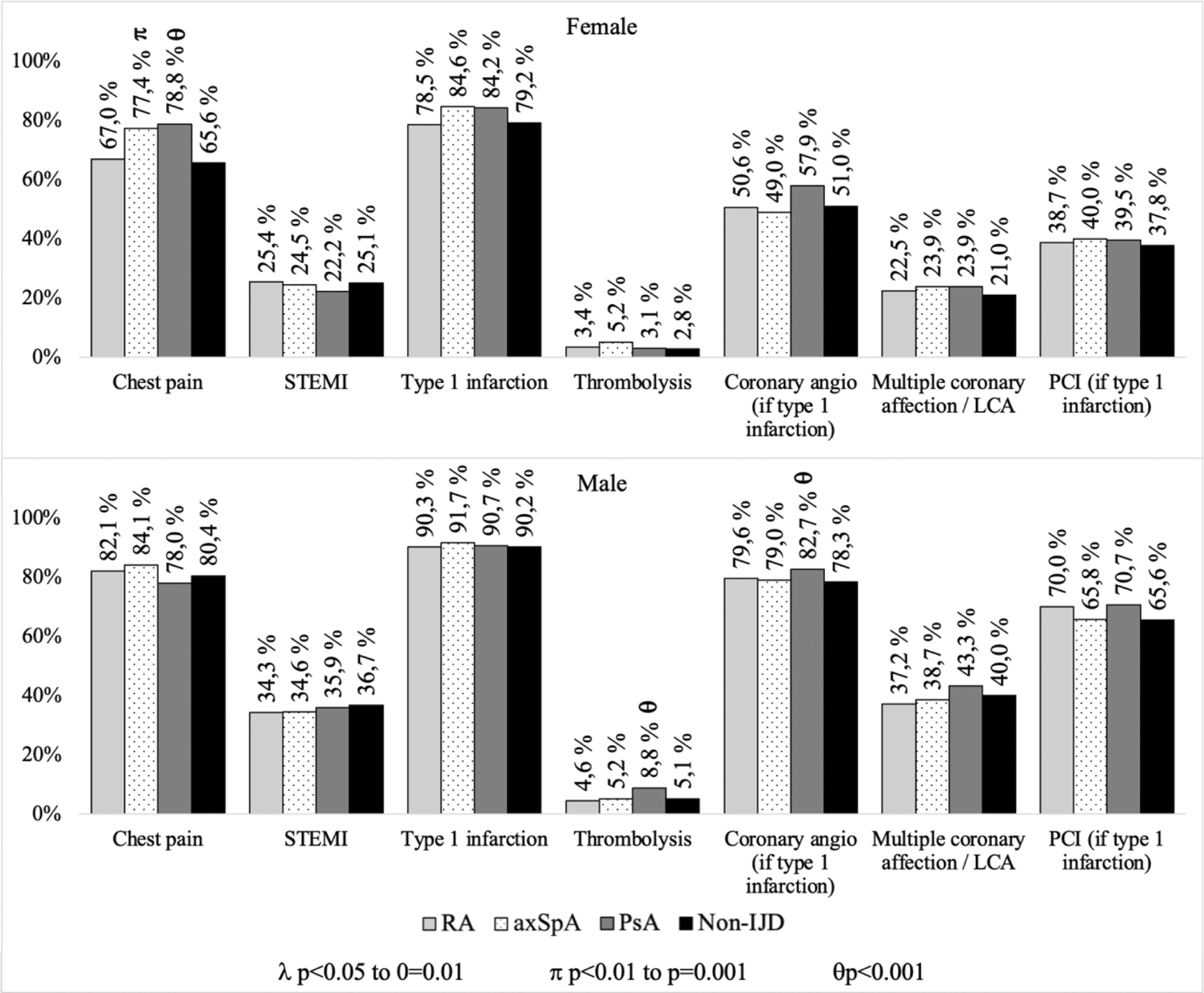
Results: Between January 2013 and December 2017, we identified 981 RA patients, 314 axSpA patients, 434 PsA patients and 34,783 non-IJD individuals without pre-existing atherosclerotic CV disease experiencing their first MI. The female proportion varied from 58.9% in RA to 28.0% in axSpA. IP weighting resulted in comparable ages for both females (RA 74.6, SpA 73.2, PsA 72.1 and non-IJD 74.4 years) and males (RA 66.7, SpA 64.8, PsA 64.7 and non-IJD 65.2 years). Figure 1 illustrates that only 65.6% of female non-IJD patients reported chest pain as the dominating symptom, which was significantly lower than in female axSpA (77.4%, p<0.01) and female PsA (78.8%, p<0.001) patients. Among males, chest pain was common in all groups, ranging from 78.0% in PsA to 84.1% in axSpA patients. The rates of ST-elevation MI (STEMI) were consistent across groups, varying from 22.2% to 25.4% in female patients and 34.3% to 36.7% in males. Similarly, the rates of type 1 infarctions showed comparable patterns. There was no indication that IJD groups received less acute thrombolysis, coronary angiography or percutaneous coronary intervention (PCI) than non-IJD. In fact, male PsA patients received thrombolysis (8.8% vs 5.1%, p=0.03) and coronary angiography (82.7% vs 78.3%, p=0.02) more often than non-IJD. The rates of multiple or left coronary artery involvement were also comparable across all groups. Additionally, there were no signs of higher Troponin T levels in any of the IJD sub-groups compared to non-IJD, regardless of STEMI or non-STEMI status (data not shown). As shown in Figure 2, none of the recorded in-hospital complications following an initial MI – such as cardiopulmonary resuscitation, non-invasive ventilation/respirator treatment, cardiogenic shock, arrhythmias and need for pacemakers or implantable cardioverter defibrillators – were more common in the IJD sub-entities compared to the non-IJD group. PsA patients had lower rates of atrial fibrillation and flutter (p<0.001 for both sexes), and female axSpA patients experienced fewer net adverse cardiovascular events (NACE) than their non-IJD counterparts (p<0.001). There was also no indication of higher in-hospital or short-term mortality in IJD patients compared to non-IJD patients. Female axSpA patients had the lowest in-hospital and short-term (30-day) mortality, at 1.7% (p<0.001).
Conclusion: Our comprehensive nationwide study demonstrates that RA, axSpA and PsA patients experiencing their first MI have similar, if not better, MI clinical courses, treatment and short-term outcomes compared to non-IJD patients. Our findings provide reassurance regarding the management and prognosis of IJD patients following an initial MI, highlighting the effectiveness of current treatment protocols. These insights reinforce the importance of sustained vigilance and proactive treatment strategies in this patient population.
REFERENCES: NIL.
Characteristics and Acute Treatment of Myocardial Infarctions in RA, axSpA and PsA Patients Compared to Non-IJD Patients Experiencing Their First Myocardial Infarction.
RA: Rheumatoid arthritis, axSpA: Axial spondyloarthritis, PsA: Psoriatic arthritis, IJD: Inflammatory joint disease, STEMI: ST elevation myocardial infaction, LCA: Left coronary artery, PCI: Percutaneous coronary intervention.
p-values calculated with non-IJD as the reference.
Acknowledgements: NIL.
Disclosure of Interests: Eirik Ikdahl: None declared, Anne Kerola Novartis, Boehringer-Ingelheim, Sanofi, Abbvie, Support for attending meetings and/or travels from Abbvie, Johnson & Johnson, Peder L. Myhre Amarin, AmGen, AstraZeneca, Bayer, Boehringer-Ingelheim, Bristol Myers Squibb, Novartis, Novo Nordisk, Pharmacosmos, Roche, Sanofi, US2.ai, Vifor, Eli Sollerud: None declared, Anne Grete Semb Merck/Schering-Plough, BMS, UCB, Pfizer/Wyeth, Novartis, Sanofi.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (