

Background: Rheumatoid arthritis (RA) and Psoriatic Arthritis (PsA) are chronic inflammatory diseases associated with increased cardiovascular risk (CVR) [1, 2]. Systemic inflammation plays a key role in the development of the atherosclerotic process, leading to this increased CVR [3]. Arterial age is a surrogate marker of vascular aging, and the presence of carotid plaques allows for the assessment of cardiovascular risk [4]. Several studies have observed differences between these diseases in CVR using stratification tools.
Objectives: To assess and compare CVR in patients with RA and PsA by estimating arterial age and identifying carotid atheroma plaques.
Methods: This single-center study analyzed 61 patients diagnosed with RA (30) and PsA (31), followed up outpatient clinics at the San Cecilio Clinical University Hospital of Granada. Inclusion criteria: patients aged ≥18 years with an established diagnosis of RA or PsA who provided consent to participate in this study. The following baseline variables were collected: age, sex, ESR, CRP, BMI, non-HDL cholesterol, smoker or ex-smoker status, hypertension, and diabetes. Mean arterial age was calculated using a program based on pulse wave velocity measurements cfPWV (carotid-femoral PWV) and baPWV (brachial-ankle PWV), and carotid ultrasound was performed to determine the presence or absence of plaques. A descriptive statistical analysis was conducted, incorporating frequencies and percentages for qualitative variables, as well as central tendency measures for quantitative variables. Additionally, measures of dispersion and distribution shape were calculated. This analysis was complemented by graphical representations for enhanced visualization, including bar charts and box-and-whisker plots. To determine whether the observed differences in sample values between RA and PsA patients were statistically significant, the Chi-square test of independence was applied to categorical variables, while the Student’s t-test was used for quantitative variables, following verification of normality using the Kolmogorov-Smirnov test. For non-normal distributions, the non-parametric Mann-Whitney U test was employed. A p-value <0.05 was set as the standard for significance.
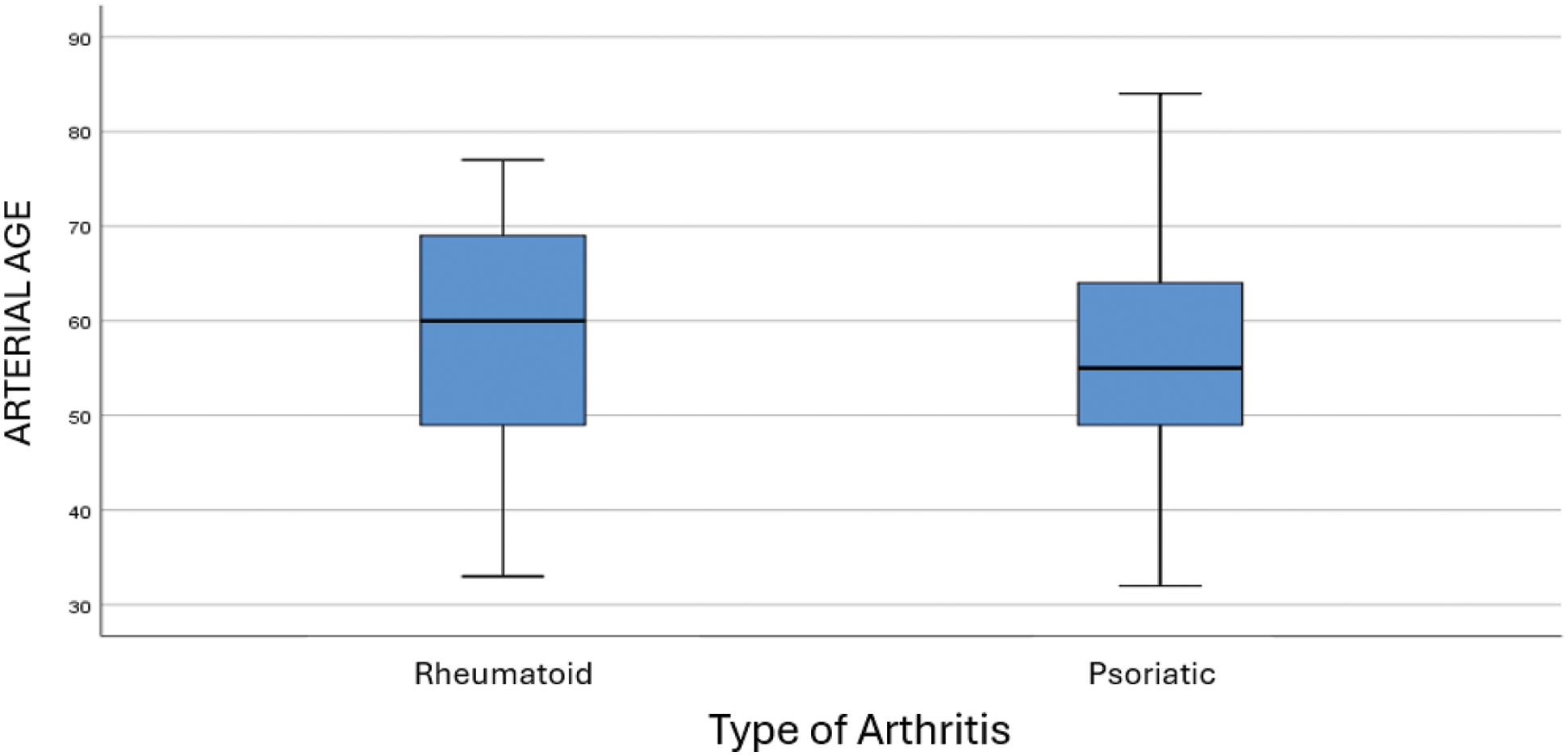
Results: Table 1 summarizes the baseline variables, arterial age and the presence of carotid atheroma plaques in the two groups. The mean arterial age was numerically higher in RA patients, with a value of 58.68 ± 12.355 years, compared to PsA patients, whose mean arterial age was 55.90 ± 12.169 years – Figure 1-. Regarding the presence of atheroma plaques, 50% of RA patients had plaques, whereas this proportion was slightly lower in PsA patients (46.4%).
Baseline characteristics, mean arterial age and percentage of carotid plaques in RA and PsA.
| Rheumatoid Arthritis (RA) | Psoriatic Arthritis (PsA) | Significant Difference | |
|---|---|---|---|
| Mean age | 59.63 ± 8.397 | 53.42 ± 9.298 | Yes (p=0.008) |
| Percentage of women | 86,7% | 41,9% | Yes (p=0.000) |
| Percentage of men | 13,3% | 58,1% | Yes (p=0.000) |
| ESR (mean) | 14.833 ± 13.170 | 14.871 ± 15.117 | No (p=0.789) |
| CRP (mean) | 4.633 ± 6.442 | 5.594 ± 7.159 | No (p=0.352) |
| BMI (mean) | 29.868 ± 6.580 | 32.655 ± 4.881 | No (p=0.065) |
| Non-HDL cholesterol (mean) | 191.60 ± 46.961 | 140.07 ± 42.654 | Yes (p=0.000) |
| Percentage of smokers/ex-smokers | 44.4% | 55.6% | No (p=0.027) |
| Percentage with hypertension | 43.6% | 56.4% | No (p=0.245) |
| Percentage with type 2 diabetes | 70.0% | 30.0% | Yes (p=0.000) |
| Mean arterial age | 58.68 ± 12.355 | 55.90 ± 12.169 | No (p=0.406) |
| Percentage with plaques | 50% | 46.4% | No (p=0.789) |
Distribution of Arterial Age by Type of Arthritis.
Conclusion: In this study, we observed that RA patients exhibited numerically higher mean arterial age and a greater prevalence of atheroma plaques compared to PsA patients. These findings suggest that RA patients have a higher atherosclerotic burden and increased cardiovascular risk compared to PsA patients. The chronic systemic inflammatory basis, along with the high prevalence of cardiometabolic comorbidities in our sample, likely contributed to the high percentage of detected carotid plaques. Therefore, we believe it is essential to prevent and control modifiable risk factors.
REFERENCES: [1] Raadsen R, Hansildaar R, Pouw LC, Hooijberg F, Boekel L, Wolbink GJ, van Kuijk AWR, Nurmohamed MT. Cardiovascular disease risk in patients with inflammatory arthritis nowadays still substantially elevated. RMD Open. 2023 Dec 1;9(4):e003485. doi: 10.1136/rmdopen-2023-003485. PMID: 38053460; PMCID: PMC10693884.
[2] Agca R, Heslinga SC, Rollefstad S, et al. EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis 2017;76:17–28.
[3] Del Rincón I, Polak JF, O’Leary DH, Battafarano DF, Erikson JM, Restrepo JF, Molina E, Escalante A. Systemic inflammation and cardiovascular risk factors predict rapid progression of atherosclerosis in rheumatoid arthritis. Ann Rheum Dis. 2015 Jun;74(6):1118-23. doi: 10.1136/annrheumdis-2013-205058. Epub 2014 May 20. PMID: 24845391; PMCID: PMC4239202.
[4] Vlachopoulos C, Terentes-Printzios D, Laurent S, et al. Association of Estimated Pulse Wave Velocity With Survival: A Secondary Analysis of SPRINT. JAMA Netw Open. 2019;2(10):e1912831. doi:10.1001/jamanetworkopen.2019.12831.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (