

Background: Patients with childhood-onset systemic lupus erythematosus (cSLE) have a higher prevalence of depression compared to healthy peers. Patients with cSLE have a 10% greater risk of major depressive disorder (MDD) compared to those with adult-onset SLE (39% vs. 29%). There is also a high prevalence of anxiety in approximately 35% of patients with cSLE. Genetics play a role in mood disorders and SLE susceptibility. There is a significant overlap between the genetics of depression and anxiety. Genome-wide association studies (GWAS) have identified >100 genetic risk loci for each of depression, anxiety and SLE. The cumulative effects of these variants can be combined into polygenic risk scores (PRS).
Objectives: Our study aims to test the association between genetic risk variants for (1) SLE (HLA and non-HLA) and (2) MDD with depression and anxiety, in a multi-ancestral cohort of children and adolescents with SLE.
Methods: We included patients followed in a tertiary care Lupus clinic from January 1, 2000, to December 31, 2023. All patients met ≥4 American College of Rheumatology (ACR) and/or Systemic Lupus International Collaborative Clinics (SLICC) criteria for SLE with data prospectively collected in a dedicated lupus database. Patients were genotyped on an Illumina multiethnic array, with un-genotyped single nucleotide polymorphisms (SNPs) imputed using TopMed as a referent. Ancestry was genetically inferred using principal components (PCs) and ADMIXTURE. We calculated additive, weighted PRSs for: 1) SLE (HLA and non-HLA) and 2) MDD using risk SNPs from the largest GWAS to date. Since there is a significant genetic overlap between depression and anxiety, we included both depression and anxiety as outcomes. We identified patients with depression and anxiety as those with a clinical diagnosis and/or persistent symptoms over two or more months, prior to or following SLE diagnosis. We tested the association between each PRS and 1) depression only, 2) anxiety only, 3) depression and anxiety, 4) depression and/or anxiety in univariate and multivariable-adjusted logistic regression models, adjusted for sex and 5 PCs (P<0.0.017). We additionally carried out sensitivity analyses focusing only on patients with a clinical diagnosis for depression and/or anxiety. We also carried out sensitivity analyses which additionally adjusted for neuropsychiatric lupus (NPSLE) status. We also tested the association between NPSLE and each outcome.
Results: Our study included 488 patients, 84% were female, with a median age of SLE diagnosis of 14 years (IQR: 12-16; Table 1). The majority of patients were of European (29%) and East Asian (27%) ancestry. The most common SLE clinical features included arthritis (68%), followed by lupus nephritis (39%) and NPSLE (21%). There were 96 (20%) patients with either a depression and/or anxiety clinical diagnosis: 28 (6%) with depression only, 25 (5%) with anxiety only, and 43 (9%) with both depression and anxiety. 181 (37%) patients had depression and/or anxiety persistent symptoms: 138 (28%) with depression only, 4 (1%) with anxiety only, and 39 (8%) with both depression and anxiety. We did not observe a significant association between PRSs for either SLE (HLA and non-HLA) or MDD and depression or anxiety (Table 2). Sensitivity analyses demonstrated similar associations between the PRSs and outcomes. NPSLE was significantly associated with depression clinical diagnosis (OR 3.89, 95% CI 2.26-6.68; P<0.001), and depression and/or anxiety (OR 2.74, 95% CI 1.70-4.52; P<0.001) in univariate and multivariable models adjusted for sex, with all estimates derived from the adjusted models.
Conclusion: In a multi-ancestral cohort of children and adolescents with SLE, we did not observe a significant association between genetic loci for SLE and MDD and depression or anxiety. This may be due to the limited generalizability of European SLE and MDD risk loci to a multi-ancestral population. Our cohort is comparable to prior studies of mood in cSLE as we found a significant association between NPSLE and depression. Future work will examine genetic variants for anxiety.
REFERENCES: NIL.
Table 1. Demographic and clinical characteristics of the cohort (n=488)
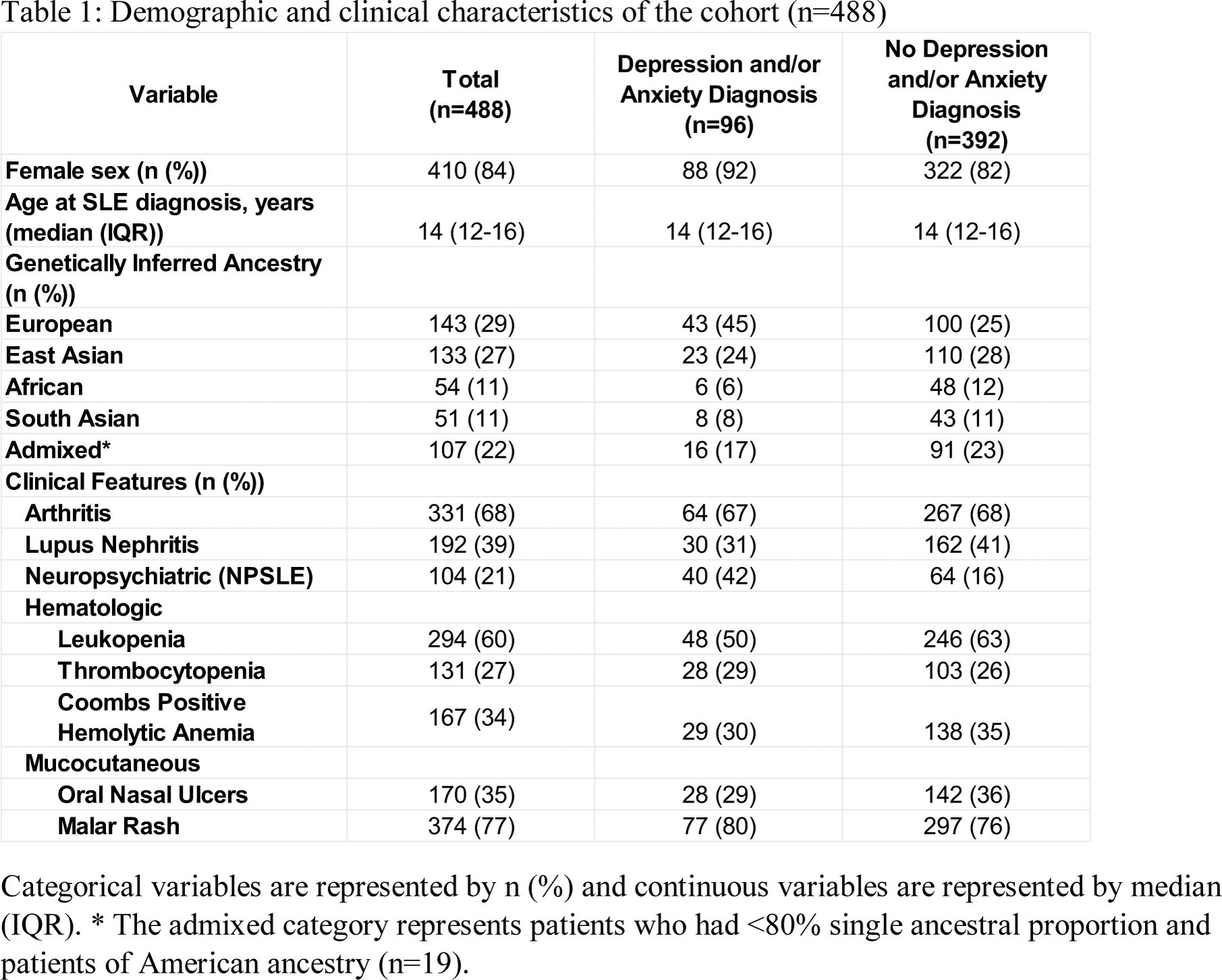
Categorical variables are represented by n (%) and continuous variables are represented by median (IQR). * The admixed category represents patients who had <80% single ancestral proportion and patients of American ancestry (n=19).
Table 2. Univariate and multivariable logistic regressions (n=488)
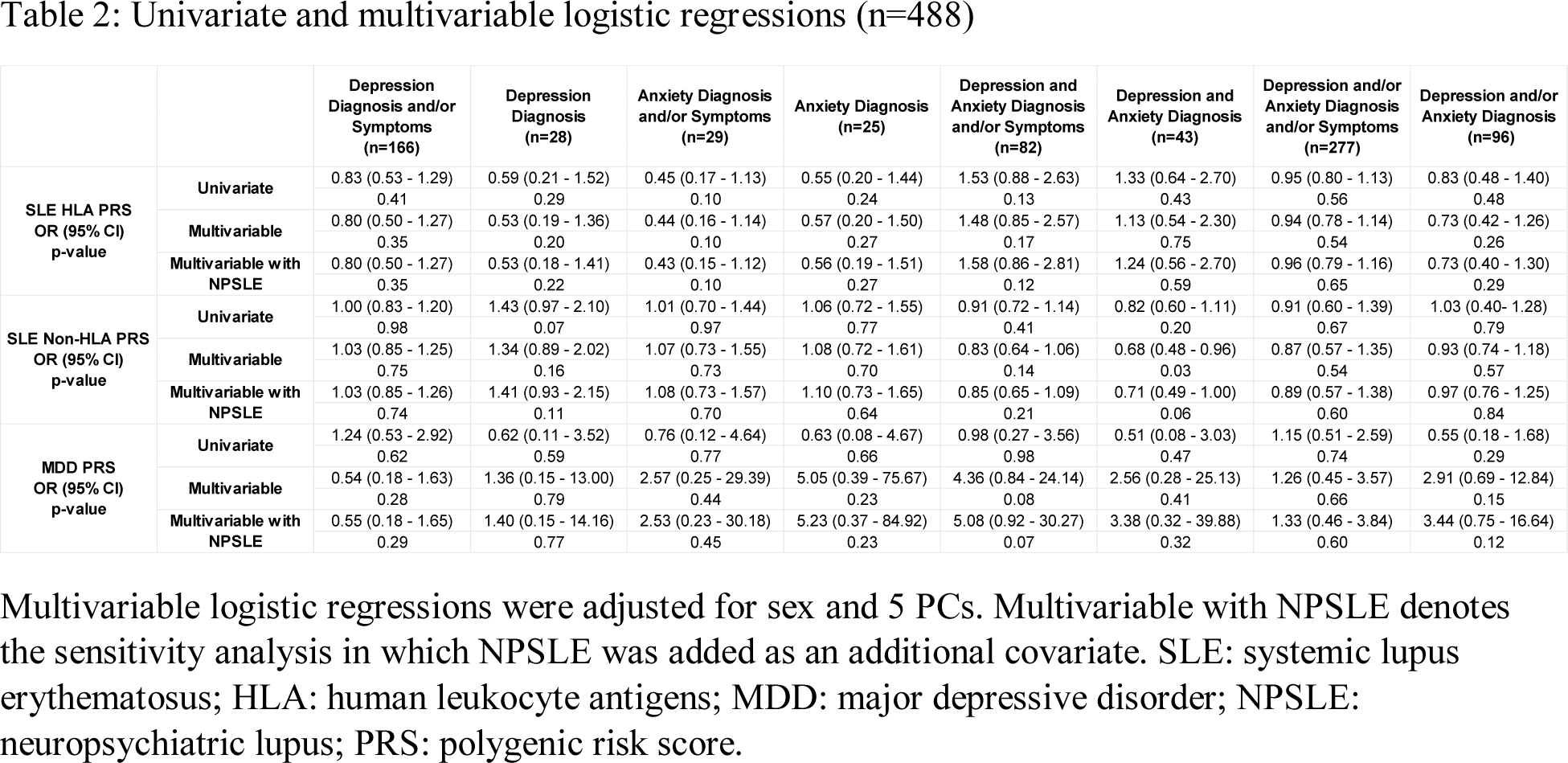
Multivariable logistic regressions were adjusted for sex and 5 PCs. Multivariable with NPSLE denotes the sensitivity analysis in which NPSLE was added as an additional covariate. SLE: systemic lupus erythematosus; HLA: human leukocyte antigens; MDD: major depressive disorder; NPSLE: neuropsychiatric lupus; PRS: polygenic risk score.
Acknowledgements: NIL.
Disclosure of Interests: Indrani Das: None declared, Alicia Tran: None declared, Nicholas Gold: None declared, Christie Burton: None declared, Jennifer Crosbie: None declared, JingJing Cao: None declared, Daniela Dominguez: None declared, Sefi Kronenberg: None declared, Deborah M Levy: None declared, Lawrence Ng: None declared, Alene Toulany: None declared, Hiu-Ki Rachel Tran: None declared, Gwyneth Zai: None declared, Andrea Knight Pfizer, Linda Hiraki Janssen.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (