

Background: Axial spondyloarthritis (axSpA) is associated with accelerated atherosclerosis driven by chronic inflammation [1]. Achieving LDA may result in significant benefits in articular disease, little is known about its effect on extra-articular disease, including cardiovascular (CV) risk in axSpA.
Objectives: To investigate the effect of achieving axial spondyloarthritis Disease Activity Score (ASDAS) low disease activity (LDA) using a protocolized treatment strategy on the progression of subclinical atherosclerosis and arterial stiffness in axSpA patients.
Methods: One hundred consecutive AxSpA patients who fulfilled the Assessment of SpondyloArthritis international Society (ASAS) criteria and active disease (ASDAS ≥2.1) participated in this 2-year prospective, hospital-based, cohort study. All participants received 24 months of tight-control treatment. Treatment was adjusted according to a standardized protocol every 3-6 monthly aiming at ASDAS LDA (ASDAS <2.1). Carotid intima-media thickness (IMT) and total plaque area (TPA) was measured using high-resolution ultrasound. The progression of carotid plaque was defined as an incident plaque in a segment without plaque at baseline, or an increased number of plaques in a segment at 24 months. Arterial stiffness was measured using pulse wave velocity (PWV) by a dedicated tonometry system and augmentation index (AIx) by the SphygmoCor device. The inflammatory burden was measured by cumulative averages of the area under the curve for ASDAS (ca-ASDAS) over a period of 2 years. The primary outcome measure was the effect of achieving LDA (LDA group) at 12 months on the progression of subclinical atherosclerosis over a period of 24 months as evaluated by IMT and TPA compared to those who cannot achieve LDA (non-LDA group). Secondary outcomes included: 1. differences in AIx and PWV progression between the LDA group and non-LDA group; 2. change in subclinical atherosclerosis and arterial stiffness makers over 24 months, comparing between patients who achieve sustained LDA (sLDA) (sLDA group: maintained LDA from 12 to 24 months) to those who did not achieve sLDA (non-sLDA group); and 3. relationship between ca-ASDAS and changes in subclinical atherosclerosis and arterial stiffness markers over a period of 24 months.
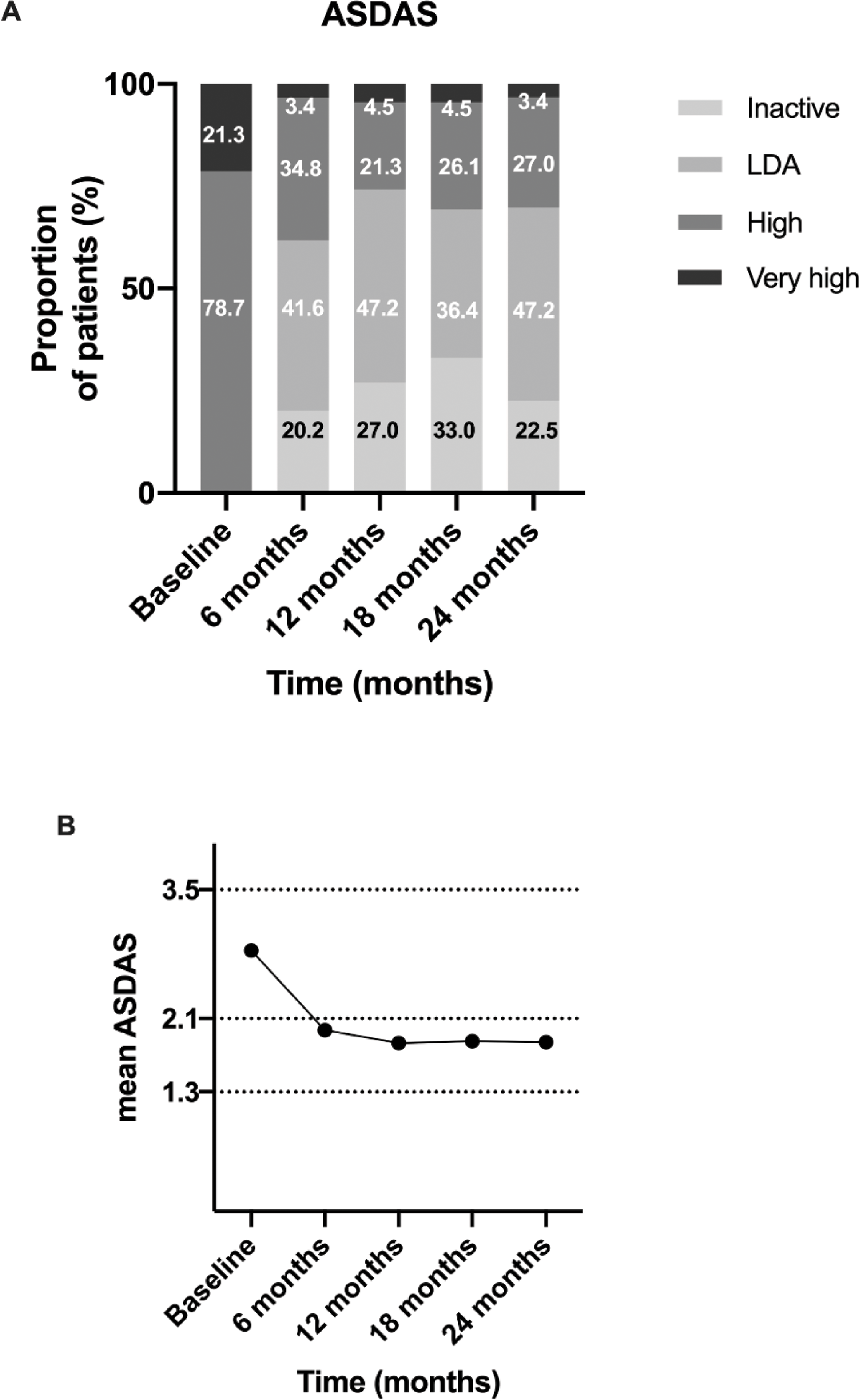
Results: A total of 89 patients with axSpA were included in this analysis, with a mean age of 39 ± 10 years, and 79.8% were male (n = 71). Over a period of 24 months, a significant improvement in disease activity was observed (ASDAS at baseline: 3.0±0.6 vs. 1.9±0.7 at 24 months, P <0.001). Sixty-six patients (74.2%) had achieved LDA at 12 months (Figure 1). At 24 months, subclinical atherosclerosis and arterial stiffness outcomes were similar between the LDA and non-LDA groups. Forty-three patients (48.3%) attained sLDA Baseline traditional CV risk factors were comparable between the sLDA and non-sLDA groups. The mean (standard deviation) change in TPA was 0.22±2.87 and 2.07±4.68 ( P = 0.034) for the sLDA group and the non-sLDA group respectively. Multivariate analysis revealed that the sLDA group experienced less progression in TPA (relative risk [RR] = -1.63 [95% confidence interval: -3.22 to -0.04], P = 0.044) after adjusted for covariates, compared to the non-sLDA group (Table 1). However, there were no significant differences in the progression of IMT and arterial stiffness markers between the two groups. Ca-ASDAS was significantly correlated with the progression of carotid plaque (rho = 0.222, P = 0.036) and TPA change at 24 months (rho = 0.225, P = 0.034).
Conclusion: Patients with AxSpA who achieved sLDA through a protocolized treatment algorithm experience less progression in TPA compared to patients who did not achieve sLDA. This suggests that effectively suppressing inflammation in AxSpA patients who attain sLDA may lower CV risk by preventing progression of subclinical atherosclerosis.
REFERENCES: [1] Gonzalez-Juanatey C, Vazquez-Rodriguez TR, Miranda-Filloy JA, Dierssen T, Vaqueiro I, Blanco R, et al. The high prevalence of subclinical atherosclerosis in patients with ankylosing spondylitis without clinically evident cardiovascular disease. Medicine (Baltimore). 2009;88(6):358-65.
(A) Disease activity state according to Ankylosing Spondylitis Disease Activity Score (ASDAS) and (B) mean ASDAS changes across the study. LDA, low disease activity.
Multivariable analysis on ASDAS sustained low disease activity (sLDA) and the progression of total carotid plaque area.
| Multivariate analysis | ||
|---|---|---|
| RR (95% CI) | P | |
| Change in total plaque area # | ||
| NSAIDs use during follow up | -3.58 (-7.04 to -0.11) | 0.043* |
| AxSpA symptom duration † | 0.12 (0.01 to 0.22) | 0.026* |
| Achieved sLDA | -1.63 (-3.22 to -0.04) | 0.044* |
*Statistically significant at P < 0.05.
† AxSpA symptom duration: the duration between axSpA symptom onset and diagnosis date.
# Adjusted for baseline tender joint count, axSpA symptom duration and nonsteroidal anti-inflammatory drugs (NSAIDs) use during follow up.
RR: relative risk; CI: confidence interval.
Acknowledgements: Project Funding Source: Health and Meidical Research Fund (HMRF), Ref no: 08190456.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (