

Background: Recent studies have suggested that autophagy may play different roles in the pathogenesis of rheumatoid arthritis (RA) and psoriatic arthritis (PsA). Lysosome-associated membrane protein type 2A (LAMP2A) is a key component of the chaperone-mediated autophagy (CMA) machinery [1]. LAMP2A may be differently regulated in RA and PsA synovial tissue. This study aims to evaluate the expression of LAMP2A and two key components of macroautophagy (ATG7, Beclin1) in synovial tissue as potential biomarkers to distinguish PsA from RA.
Objectives: The primary objective of this study is to assess the expression of LAMP2A, ATG7 and Beclin1 in synovial tissue and evaluate their potential as biomarkers for differentiating between PsA and RA.
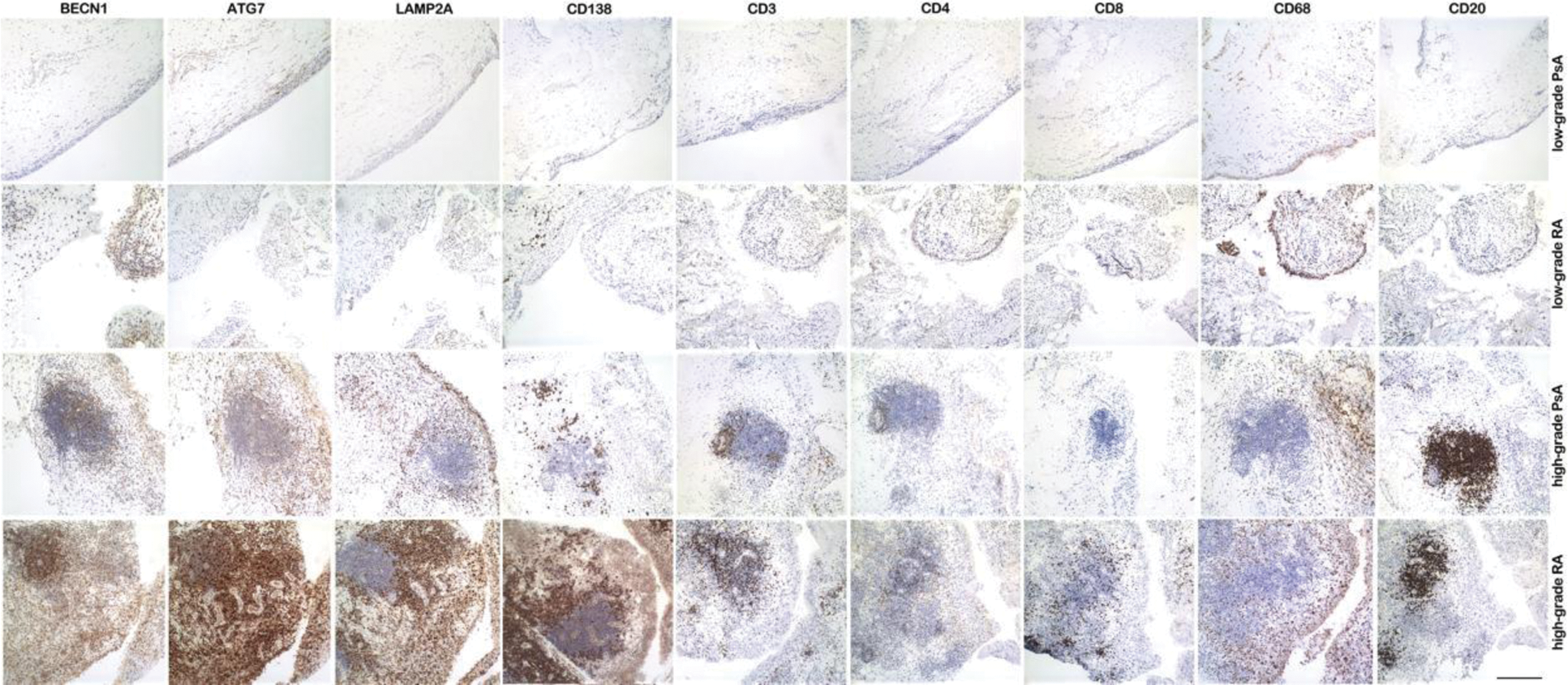
Methods: This study included patients with classified PsA and RA who underwent ultrasound-guided synovial biopsy. Synovial specimens were stained with hematoxylin and eosin (H&E) for Krenn’s synovitis score and immunohistochemically stained with antibodies against CD3, CD4, CD8, CD20, CD138, LAMP2A, ATG7 and Beclin1. Positivity for each marker was quantified using ImageJ software on microphotographs. The density of LAMP2A-positive, ATG7-positive and Beclin1-positive cells (n/mm2) was counted in the synovial lining layer, synovial stroma, and inflammatory infiltrate. Comparisons between PsA and RA were performed using t-tests, also stratifying by Krenn’s synovitis grading. Logistic regression analysis was employed to evaluate the ability of LAMP2A-positive and ATG7-positive cell density to discriminate between RA and PsA, with the area under the receiver operating characteristic curve (AUROC) used to assess diagnostic performance.
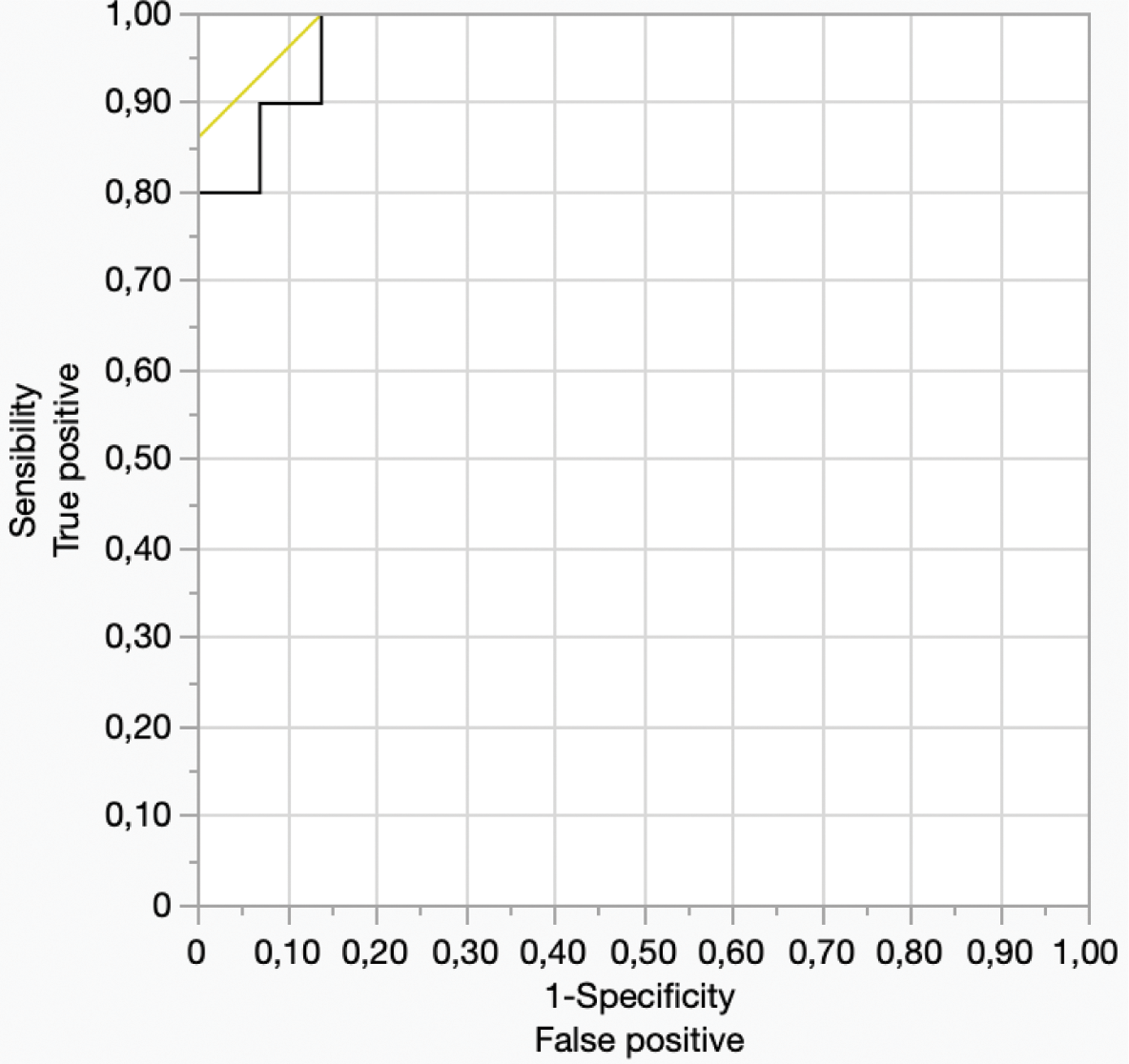
Results: The study included 29 PsA patients (mean age 50.53 ± 12.02 years; mean DAPSA score 17.25 ± 4.63 at biopsy) and 11 RA patients (mean age 53.31 ± 9.31 years; mean DAS28 score 4.36 ± 1.05 at biopsy). Nineteen (65.52%) PsA synovial specimens had high-grade synovitis (Kreen score ≥ 5), while six (54.55%) synovial specimens showed high-grade synovitis. LAMP2A-positive cell density in the synovial lining layer was similar between PsA and RA patients (p=0.26), regardless of synovitis grade. In the synovial stroma, LAMP2A-positive cell density trended towards a difference between PsA and RA (p=0.08). In high-grade synovitis, RA specimens had higher LAMP2A-positive cell density than PsA patients (p=0.03). LAMP2A-positive cell density in the inflammatory infiltrate was significantly different between PsA and RA patients (Figure 1), with RA specimens displaying higher density than PsA (p=0.0001). This difference was also observed in low-grade synovitis (RA vs. PsA, p=0.008). Logistic regression analysis demonstrated that the density of LAMP2A-positive cells in the inflammatory infiltrate could differentiate RA from PsA after adjusting for synovitis grade (OR 1.02, 95% CI 1.01-1.03), with an AUC of 0.89. Moreover, ATG7-positive cell density (Figure 1) was significantly higher in RA compared to PsA in the synovial lining layers (p=0.0529; high-grade: p=0.0018), synovial stroma (p=0.0356), and inflammatory infiltrate (p<0.0001; low-grade: p=0.011; high-grade: p=0.0004). The density of ATG7 in the inflammatory infiltrate could also differentiate RA from PsA (OR 1.07, 95% CI 1.01-1.13) with an AUC of 0.95, after adjusting for synovitis grade. On the other end, no significant differences were observed in Beclin1-positive cell density in synovial tissues between RA and PsA cases. The combination of LAMP2A and ATG7 inflammatory infiltrate density further improved the discriminative ability between RA and PsA, with LAMP2A emerging as the independent predictor of diagnosis (OR 1.021, 95% CI 1.003-1.040) with an AUC of 0.98 (Figure 2).
Conclusion: This study demonstrates that LAMP2A and ATG7 expression in the inflammatory infiltrate of synovial tissue is significantly higher in RA compared to PsA, regardless of the synovitis grade. Moreover, LAMP2A emerged as the critical discriminating factor regardless of synovitis grade. These results highlight a possible predominant role of CMA over macroautophagy in distinguishing RA from PsA in synovial biopsies and provide novel insights into the potential role of LAMP2A inflammatory infiltrate density as a novel biomarker for differential diagnosis.
REFERENCES: [1] Kaushik, S., Cuervo, A.M. The coming of age of chaperone-mediated autophagy. Nat Rev Mol Cell Biol 19 , 365–381 (2018).
CD68 + sublining macrophages, plasmacells and T-lymphocytes seems to display a stronger LAMP2A and ATG7 positivity in RA patients, regardless of synovitis grading
The combination of LAMP2A and ATG7 inflammatory infiltrate density further improved the discriminative ability between the two diseases. AUC=0.98
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (