

Background: Juvenile Idiopathic Arthritis (JIA) is a chronic inflammatory rheumatic disease prevalent in children, with an immunological basis in its etiopathogenesis [1]. Barriers to physical activity (PA) in this population significantly hinder exercise adherence [2]. In the literature, it is emphasized that digital health applications should be designed more systematically and tailored to increase participation in PA promotion and regular exercise programs [3]. Furthermore, comparative studies are needed to demonstrate their effectiveness in patients with JIA. However, no studies have compared the effectiveness of a personalized mobile application-based exercise program with a supervised personalized exercise program in JIA patients.
Objectives: The aim of the study was to compare the effectiveness of a personalized mobile-based exercise program, utilizing a data-driven artificial intelligence (AI) model, with a physiotherapist-supervised personalized exercise program on functional capacity, physical fitness and walking parameters in adolescents with JIA.
Methods: Seventeen adolescents with JIA (14 females, 3 males; aged 12-18) participated in this study, divided into two groups. First group (n:7) engaged in a personalized exercise regimen delivered through the Pediatric Physical Activity Tracking Platform (Pedi@ctivity) mobile application with a data-driven AI model (M-Health). The other group (n:10) received a personalized exercise program created by the Pedi@ctivity analysis app applied under the supervision of a physiotherapist in a clinical setting 2 days a week and online synchronously 1 day a week (SuperEx). Both programs applied for 40-45 minutes per session, three times a week over 12 weeks. Gait parameters were evaluated with the Smart Insole System. Functional capacity was assessed using the 6-Minute Walking Test (6MWT), 10 Stair Climb Test (10SCT) and 1-Minute Sit-to-Stand Test (1MSTST), and Physical fitness was measured using subtests from the FitnessGram Physical Activity Test Battery as Curl-up Test (CUT) for trunk muscle strength and endurance, Trunk Lift Test (TLT) for trunk flexibility, Push-up Test (PUT) for upper extremity muscle strength and endurance, Back Saver and Reach Test (BRT) for lower extremity flexibility and Progressive Aerobic Cardiovascular Endurance Run (PACER) for aerobic endurance. The results of each test were evaluated and categorized in terms of health risk according to age (Needs Improvement (NI)-Health Risk, NI and healthy fitness zone (HFZ)). Besides, the 6MWT and 1MSTST scores were also categorized using age-matched healthy reference values. Participants used smartwatches during the programs to monitor health-related parameters and physical activity behaviors, with data recorded in the Pedi@ctivity app. Evaluations were conducted at baseline (T1) and after 12 weeks (T2).
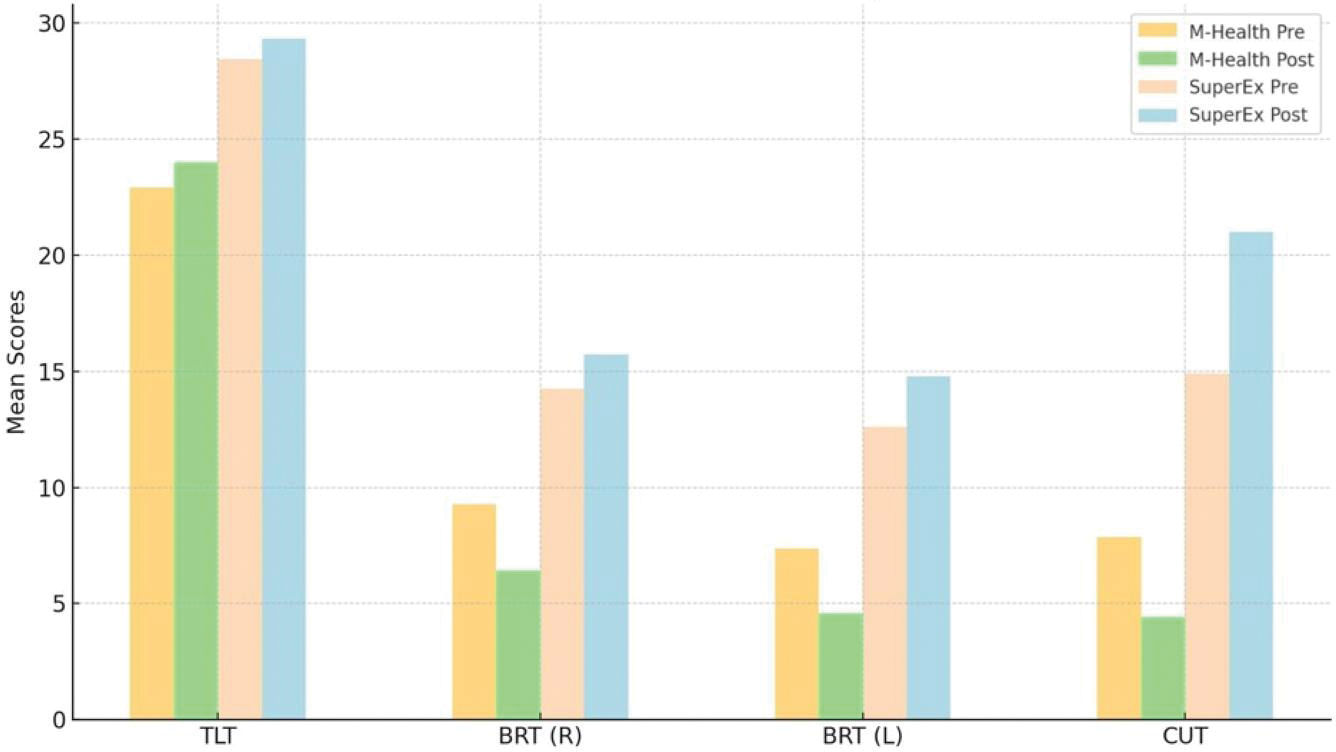
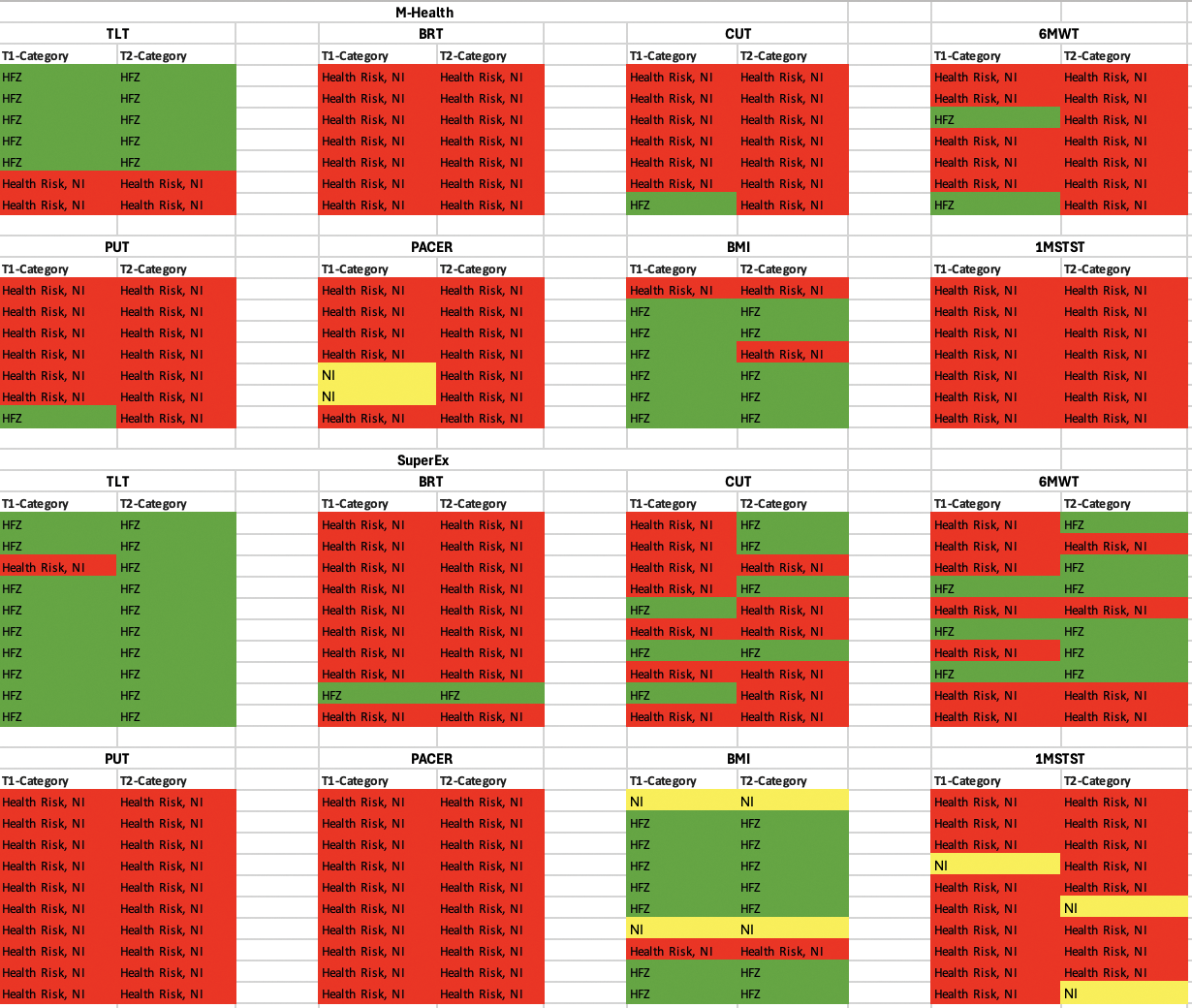
Results: The mean age of the M-Health participants was 13.43±0.97 and SuperEx was 14.80±2.34 years. At T1, there were no significant differences between the groups in almost all outcome measures (p>0.05), except for the TLT (p<0.05). When examining within-group T1-T2 differences, a significant increase in walking speed (m/s) was observed in both groups (p<0.05). In the intergroup analysis, significant differences were found in the CUT, TLT, and BRT (right (R)-left (L)) scores at T2, favoring SuperEx (p<0.05) (Figure 1). In the intragroup analysis, the category differences of the FitnessGram, for T1-T2, in the CUT and 6MWT categories, the number of adolescents classified within the HFZ increased from 3 at T1 to 4 and 6 at T2, respectively. In the 1MSTST categories, the number of individuals meeting the initial percentile threshold rose from 1 at T1 to 2 at T2 (Figure 2).
Conclusion: This pilot study demonstrated that both a data-driven AI-based exercise program and a physiotherapist-supervised AI-based program improved physical fitness and walking parameters in adolescents with JIA. Increased walking speed in both groups highlights the potential to enhance overall physical performance, possibly influenced by higher PA engagement through smartwatch use. Greater improvements in trunk strength, endurance, and flexibility were observed in the supervised group (SuperEx), likely due to motivational support provided by direct supervision. However, the smaller M-Health sample size may have contributed to these differences. Moreover, significant improvements in physical fitness parameters were not consistently reflected in health risk categorizations. This may be due to the FitnessGram may not be sensitive enough to reveal changes in physical fitness because the range of categories in the score is wide and it was designed for healthy children rather than adolescents with chronic diseases such as JIA. In conclusion, this study is the first to compare supervised and mobile-delivered AI-based exercise approaches tailored for adolescents with JIA, supporting physical fitness and walking performance. Future research should explore long-term effects and program adaptability for various age groups and health conditions.
REFERENCES: [1] Petty, RE., et al. 2005. “Chronic arthritis.” Textbook of Pediatric Rheumatology.
[2] Griffiths, AJ., et al. 2018. “The effect of interactive digital interventions on physical activity in people with inflammatory arthritis: a systematic review”, Rheumatol Int.
[3] Butler, S., et al. 2022. “Effectiveness of eHealth and mHealth Interventions Supporting Children and Young People Living with Juvenile Idiopathic Arthritis: Systematic Review and Meta-analysis”, J Med Internet Res.
Pre (T1) -Post (T2) comparison of FitnessGram test scores for both groups
Pre (T1) -Post (T2) FitnessGram categories for both groups
BMI: Body Mass Index
Acknowledgements: This study was supported by Scientific and Technological Research Council of Turkey (TUBITAK) under the Grant Number 124S137. The authors thank to TUBITAK for their supports.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (