

Background: Primary Sjögren’s Syndrome (pSS), the second most common rheumatic disease, remains a clinical challenge due to inconclusive evidence regarding its pharmacologic and non-pharmacologic management strategies [1, 2]. Although EULAR guidelines emphasize the benefits of exercise in managing inflammatory arthritis and osteoarthritis [3, 4], the specific effects of exercise interventions on pSS remain insufficiently explored, revealing a critical gap in the management of pSS.
Objectives: This systematic review and meta-analysis aimed to evaluate the effects of exercise interventions on key outcomes in pSS, including dryness, fatigue, pain, quality of life, disease activity, and aerobic capacity. Additionally, the review sought to identify the most effective type of exercise to optimize patient outcomes.
Methods: This systematic review was conducted in accordance with the PRISMA Statement and was registered on PROSPERO (CRD42024540641). Six databases (Web of Science, PubMed/MEDLINE, ProQuest, SCOPUS, Cochrane Library, and PEDro) were systematically searched up to April 2024 without restrictions. We included randomized clinical trials (RCTs) exploring the effects of exercise interventions in adult patients with pSS. Screening, data extraction, and quality assessment of eligible trials were independently performed by two researchers. Methodological quality was evaluated using the Risk of Bias version-2 tool (RoB2) and the PEDro scale. A random-effects meta-analysis was performed to calculate pooled effect sizes and 95% confidence intervals (CIs).
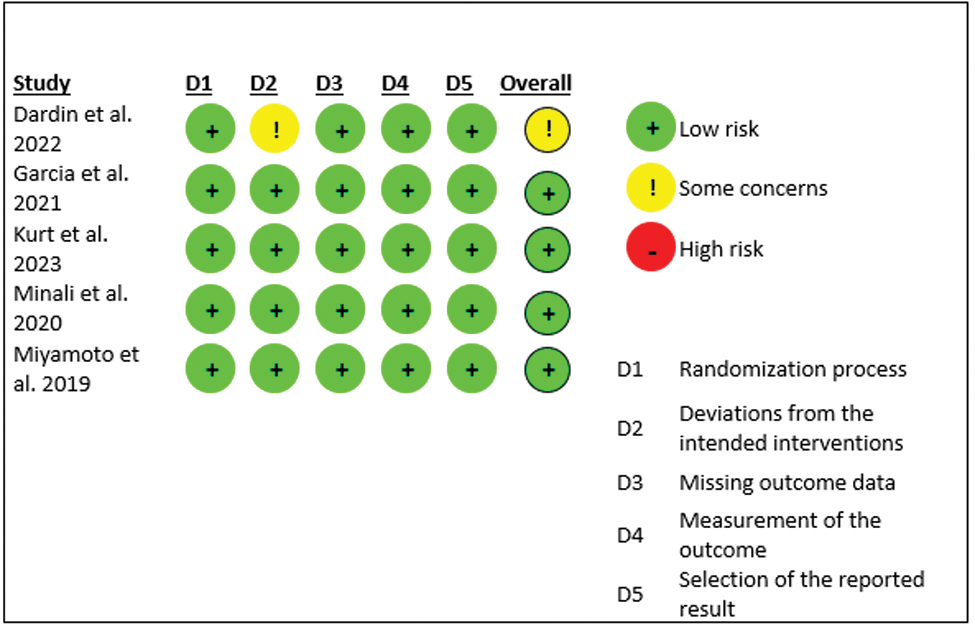
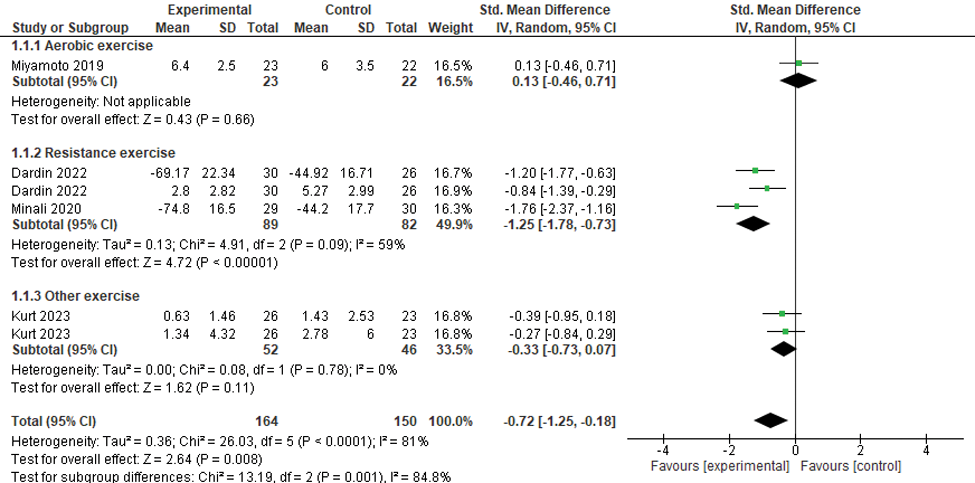
Results: A total of 744 studies were initially screened, with five randomized controlled trials (RCTs) ultimately included in the final analysis, encompassing 269 female patients aged 18 years and older diagnosed with primary Sjögren’s syndrome (pSS). The interventions evaluated included aerobic exercise, resistance exercise, combined aerobic and resistance exercise, and pelvic floor training, compared against a no-treatment control group. The risk of bias (RoB2) assessment for the included studies ranged from low risk to some concerns, as illustrated in Figure 1. Methodological quality, assessed using the PEDro scale, revealed a score of 7/10 for one study and 8/10 for the remaining four studies. The pooled analyses indicated that exercise interventions significantly improved pain (SMD -0.72; 95% CI -1.25, -0.18; p = 0.008; I² = 81%), fatigue (SMD -0.89; 95% CI -1.21, -0.58; p < 0.00001; I² = 59%), quality of life (SMD -0.55; 95% CI -0.85, -0.25; p = 0.0003; I² = 50%), and aerobic capacity (SMD -0.27; 95% CI -0.48, -0.07; p = 0.009; I² = 0%) compared to controls. No significant improvements were observed for disease activity (MD -0.74; 95% CI -2.25, 0.77; p = 0.34; I² = 49%) and dryness (MD 0.10; 95% CI -1.41, 1.60; p = 0.90; I² = 0%). Subgroup analyses indicated that resistance exercise was particularly effective, showing significant improvements in pain (SMD -1.25; 95% CI -1.78, -0.73; p < 0.00001), fatigue (SMD -1.07; 95% CI -1.34, -0.80; p < 0.00001), quality of life (SMD -0.78; 95% CI -1.05, -0.51; p < 0.00001), and disease activity (MD -1.36; 95% CI -2.48, -0.25; p = 0.02). Aerobic capacity was most improved by a combination of aerobic and resistance exercises (SMD -0.45; 95% CI -0.79, -0.11; p = 0.01; I² = 24%).
Conclusion: This systematic review and meta-analysis provides evidence supporting the significant benefits of exercise interventions in reducing pain and fatigue as well as enhancing quality of life and aerobic capacity for patients with pSS. These findings underscore the critical role of structured exercise programs as part of non-pharmacological management strategies for pSS. Nonetheless, further high-quality RCTs with larger sample sizes are necessary to strengthen the certainty of these findings and guide future clinical recommendations.
REFERENCES: [1] Fox RI, Fox CM, Gottenberg JE, Dörner T. Treatment of Sjögren’s syndrome: current therapy and future directions. Rheumatology 2021;60(5):2066-74.
[2] Ramos-Casals M, Brito-Zerón P, Bombardieri S, et al. EULAR recommendations for the management of Sjögren’s syndrome with topical and systemic therapies. Annals of the rheumatic diseases 2020;79(1):3-18.
[3] Geenen R, Overman CL, Christensen R, et al. EULAR recommendations for the health professional’s approach to pain management in inflammatory arthritis and osteoarthritis. Annals of the rheumatic diseases 2018;77(6):797-807.
[4] Santos EJF, Farisogullari B, Dures E, Geenen R, Machado PM. Efficacy of non-pharmacological interventions: a systematic review informing the 2023 EULAR recommendations for the management of fatigue in people with inflammatory rheumatic and musculoskeletal diseases. RMD open 2023;9(3):e003350.
Risk of bias graph: review authors’ judgments about each risk of bias item presented as percentages across all included studies utilizing intention-to-treat analysis.
Forest plot of pain scores for exercise vs control.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (