

Background: Chronic low back pain (CLBP) is a prevalent issue affecting a significant portion of the population. Literature indicates that some individuals with CLBP may have inflammatory causes, particularly axial spondyloarthritis (axSpA) [1]. However, axSpA can take up to 13 years to be diagnosed and significantly affects patients’ quality of life [2]. Early diagnosis and treatment of axSpA are crucial to preventing disease progression and improving quality of life. Physiotherapists play a vital role in the evaluation and management of patients with back pain. Awareness of inflammatory low back pain is essential in reducing diagnostic delays in conditions like axSpA [3].
Objectives: This study aimed to evaluate the awareness levels, treatment approaches, and clinical decision-making processes of physiotherapy students regarding inflammatory low back pain and other types of back pain.
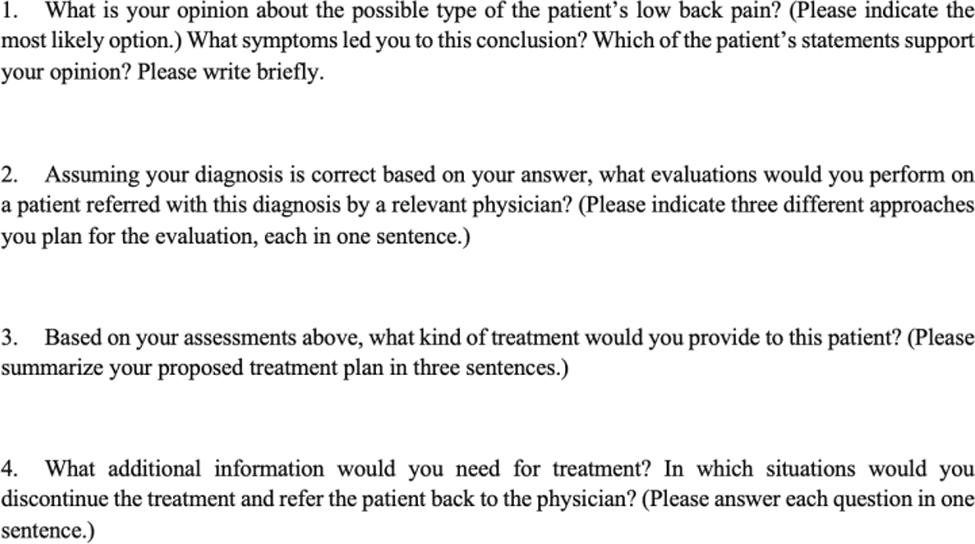
Methods: The study included senior physiotherapy students who had completed internships in at least five different departments. Participants were asked to complete an online survey that assessed their demographic characteristics, clinical experience, and clinical decision-making skills for managing low back pain cases. Participants were asked to rate their level of difficulty in clinical decision-making and their competence in clinical decision-making on a scale from 0 to 10. The difficulty level reflected how challenging they found making decisions in the cases, while the competence score represented their confidence in their clinical decision-making skills. The survey included four detailed case scenarios specifically designed to represent lumbal disc herniation, fibromyalgia, non-spesific CLBP, and axSpA. Questions related to these cases are presented in Figure 1.
Questions participants answered for each case
Treatment approaches were categorized into different areas, including exercise and biopsychosocial interventions. The analysis highlighted differences in the management of inflammatory and non-inflammatory low back pain.
Results: A total of 25 physiotherapy students participated in the study (5 male, 20 female). The average difficulty level in decision-making was 5.28, and the mean clinical decision-making competence score was 5.56. The rates of accurate diagnosis are presented in Table 1.
Rates of accurate diagnosis by participants
| Diagnosis | Correct (%) | Alternative Plausible Diagnoses (%) | Incorrect (%) |
|---|---|---|---|
| Disc herniation | 76% | 16% | 8% |
| Fibromyalgia | 48% | 32% | 20% |
| Non-specific CLBP | 52% | 28% | 20% |
| axSpA | 16.7% | 45.8% | 37.5% |
CLBP, chronic low back pain; axSpA, axial spondyloarthritis.
Participants’ responses to the evaluation questions were generally aligned with the diagnoses; however, treatment recommendations reflected a limited approach. All participants suggested exercise interventions suitable for their presumed diagnoses. However, these recommendations often did not fully reflect a biopsychosocial perspective. Treatment preferences are summarized below: Disc Herniation: 28% of participants recommended patient education, mostly limited to ergonomic corrections and posture training. Fibromyalgia: 24% referred for psychological support, and 36% incorporated biopsychosocial interventions. Non-specific CLBP: 48% suggested patient education, with 36% focusing solely on posture training. AxSpA: Only 9% recommended biopsychosocial interventions, and 9% provided posture-based education.
Conclusion: This study highlights the critical role of physiotherapists in the early diagnosis and management of inflammatory conditions like axSpA. However, it also revealed significant gaps in physiotherapy students’ knowledge and awareness of different etiologies of back pain. While all participants proposed exercise interventions consistent with their presumed diagnoses, the biopsychosocial approach remained limited across all back pain cases. Greater emphasis should be placed on the importance of the biopsychosocial approach in managing both inflammatory and non-inflammatory low back pain during physiotherapy education [4, 5]. Future studies should focus on developing structured training programs to teach this approach effectively, thereby reducing diagnostic delays and improving patient outcomes.
REFERENCES: [1] Sieper, J., Braun, J., Dougados, M., & Baeten, D. (2015). Axial spondyloarthritis. Nature reviews Disease primers, 1(1), 1-16.
[2] Deodhar, A., Mittal, M., Reilly, P., Bao, Y., Manthena, S., Anderson, J., & Joshi, A. (2016). Ankylosing spondylitis diagnosis in US patients with back pain: identifying providers involved and factors associated with rheumatology referral delay. Clinical rheumatology, 35, 1769-1776.
[3] Steen, E., McCrum, C., & Cairns, M. (2021). Physiotherapists’ awareness, knowledge and confidence in screening and referral of suspected axial spondyloarthritis: A survey of UK clinical practice. Musculoskeletal Care, 19(3), 306-318.
[4] Alperovitch-Najenson, D., et al., WHO guideline for non-surgical management of chronic primary low back pain in adults in primary and community care settings. 2023: World Health Organization.
[5] Geenen R, Overman CL, Christensen R, et al EULAR recommendations for the health professional’s approach to pain management in inflammatory arthritis and osteoarthritis Annals of the Rheumatic Diseases 2018;77:797-807.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (