

Background: Juvenile Dermatomyositis (JDM) is a rare inflammatory myopathy in which the immune system targets the microvasculature of the skeletal muscle and skin, leading to muscle weakness and a typical skin rash. Patients with JDM usually show low lean mass and bone mass, proximal muscle weakness, reduced muscle endurance, aerobic deconditioning and severe exercise intolerance [1, 2].
Objectives: The aim of this study was to investigate the functional capacity and physical fitness levels of children and adolescents with JDM and examine the relationship between muscle strength and exercise capacity in patients with JDM.
Methods: Nine children and adolescents (4 girls, 5 boys) between the ages of 6 and 17 years diagnosed with JDM were included in this study. ‘Childhood Myositis Assessment Score’ (CMAS) was used to evaluate the functional results of proximal muscle strength and endurance. The physical fitness of the patients was evaluated by using subtests from the FitnessGram Physical Activity Test Battery (FGPATB) as Curl-up Test (CUT) for trunk muscle strength and endurance, Push-up Test (PUT) for upper extremity muscle strength and endurance, Back Saver and Reach Test (BSRT) for lower extremity flexibility and Progressive Aerobic Cardiovascular Endurance Run (PACER) for aerobic endurance. By using the “VO2calculator” application, the maximum oxygen consumption value (VO2 max) was calculated for each patient based on the number of rounds completed in PACER. The results of each test were evaluated and categorized in terms of health risk according to age (Needs Improvement (NI)-Health Risk (HR), NI and healthy fitness zone (HFZ)). Six Minute Walking Test (6MWT) and 1-Minute Sit-to-Stand Test (1MSST) were used to evaluate functional capacity.
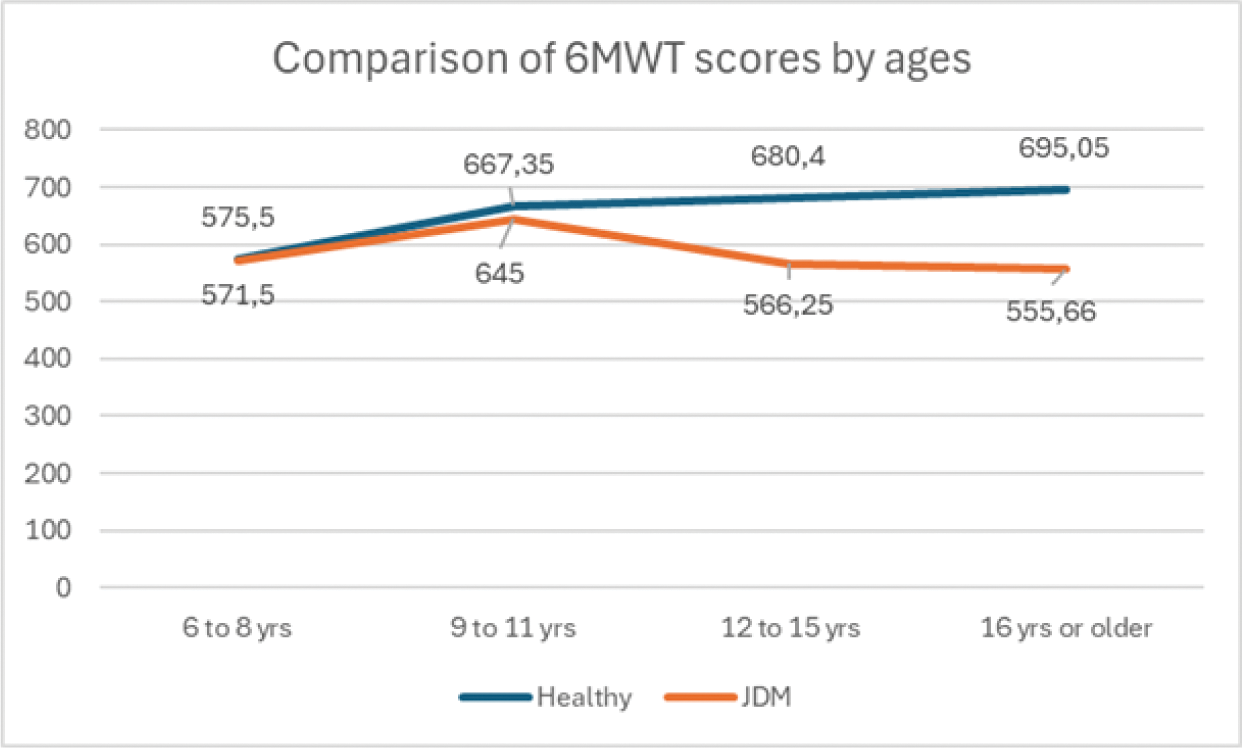
Results: The means of age and Body Mass Index (BMI) of children with JDM were 12,11±4,42 (min=6,max=17) years, 18,67±2,76kg/m 2 (min=14, max=24), respectively. Compared to the FitnessGram Health Categories Standards determined by gender and age groups, 83.3% of the children and adolescents diagnosed with JDM were in the “NI-Health Risk” and 16.7% in the “NI” category according to the VO2 max health categories, 44.4% of the patients were in the “NI” and 55.6% were in the “HFZ” category according to the CUT health categories, 44.4% of the patients were in the “HFZ” and 55.6% were in the “NI” according to the PUT health categories. In the BSRT 100% of the patients were evaluated in “NI-Health Risk” category. Individual test results for each patient are categorized according to the FitnessGram Health Categories Standards and shown in Table 1. Lower scores were found in all patients with JDM in the 1MSST compared to their healthy peers in the same percentile (mean: 26,22±7,79 min=17, max=41) [3]. The mean of the 6MWT results were 586.91±78.14 meter (min=480, max=690 meter). As shown in Figure 1, the walking distance of all JDM patients was lower than the healthy age group reference values for 6MWT [4]. CMAS showed strong correlation with CUT (r=0,83, p<0.005) and PUT (r=0,78, p <0.005). PUT also correlated with the 6MWT(r=0,83, p <0.005) and PACER (r=0,73, p <0.005).
Conclusion: In our study, it was observed that the functional capacity and physical fitness levels of children and adolescents diagnosed with JDM were significantly lower compared to the reference values for healthy children. These findings suggest that JDM has a significant impact not only on muscle strength but also on cardiovascular endurance and overall physical fitness. According to the results of this study, a relationship was found between functional muscle strength and trunk and upper extremity muscle strength in patients with JDM. Additionally, we identified a relationship between trunk muscle strength, functional capacity, and aerobic endurance. Therefore, we believe that when planning exercise programs to improve functional muscle strength and functional capacity, it is necessary to evaluate the trunk and upper extremity muscles and incorporate multimodal exercise content. More research is needed to investigate effective strategies to improve physical fitness and functional outcomes in this population.
REFERENCES: [1] Corrado, B., Ciardi, G., & Lucignano, L. (2020). Supervised Physical Therapy and Polymyositis/Dermatomyositis—A Systematic Review of the Literature. Neurology International , 12 (3), 77-88.
[2] Cheeti, A., & Panginikkod, S. (2018). Dermatomyositis and polymyositis.
[3] Haile, S. R., Fühner, T., Granacher, U., Stocker, J., Radtke, T., & Kriemler, S. (2021). Reference values and validation of the 1-minute sit-to-stand test in healthy 5–16-year-old youth: a cross-sectional study. BMJ open , 11 (5), e049143.
[4] Geiger, R., Strasak, A., Treml, B., Gasser, K., Kleinsasser, A., Fischer, V., & Stein, J. I. (2007). Six-minute walk test in children and adolescents. The Journal of pediatrics , 150 (4), 395-399.
Mean scores of 6MWT by age group
Fitnessgram health categories of all patients
| Patients | BMI | VO2 | CUT | PUT | BSRT |
|---|---|---|---|---|---|
| 1 | HFZ | NI | HFZ | HFZ | NI-HR |
| 2 | HFZ | NI-HR | HFZ | HFZ | NI-HR |
| 3 | HFZ | NI-HR | NI-HR | HFZ | NI-HR |
| 4 | HFZ | NI-HR | HFZ | HFZ | NI-HR |
| 5 | HFZ | NI-HR | NI-HR | NI-HR | NI-HR |
| 6 | NI-HR | NI-HR | HFZ | NI-HR | NI-HR |
| 7 | HFZ | NI-HR | NI-HR | NI-HR | NI-HR |
| 8 | HFZ | NI-HR | NI-HR | NI-HR | NI-HR |
| 9 | HFZ | NI-HR | HFZ | NI-HR | NI-HR |
HFZ: Healthy Fitness Zone, NI:Need Improvement, NI-HR:Need Improvement-Health Risk
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (