

Background: In Canada, an Advanced Physiotherapist Practitioner (APP) can manage complex rheumatic disease cases in shared care models [1]. These models demonstrate increased access to care, decreased wait times, and increased patient satisfaction [1]. The APP role has been studied in adult rheumatology, with less focus on pediatrics or how this role is impacted by gender [1]. Rheumatic diseases disproportionately affect women and girls – yet, there is little research on impacts to care based on gender [2]. In 2020, an APP shared care model was implemented in a pediatric rheumatology center in Ontario, Canada. The APP contributes to service delivery by assessing new consults and managing children with rheumatic diseases. Investigating patient and parent perspectives with new pediatric healthcare service delivery is imperative.
Objectives: This study aimed to i) measure and describe parent and patient satisfaction in a Canadian pediatric rheumatology center with an APP shared care model, and ii) explore differences between patient and parent responses based on gender.
Methods: This mixed-methods, cross-sectional study included all parents and patients aged 12-17 years seen by one APP in a Canadian pediatric rheumatology center (May–November 2024). Each family was a unique case with multiple responses (parent(s) and/or patient). Parent and patient demographics were collected. An adapted 9-item Visit-Specific Questionnaire (VSQ) was used to measure satisfaction with different aspects of the visit and care using a 5-point Likert scale (scores transposed to 100) and open-ended questions [3]. Parents were asked 3 additional questions to determine their opinion of the influence of gender (their own, patient, or APP) on overall satisfaction. Continuous variables (means and 95% confidence intervals) and categorical variables (frequencies and proportions) were reported. Qualitative responses were analyzed using inductive content analysis.
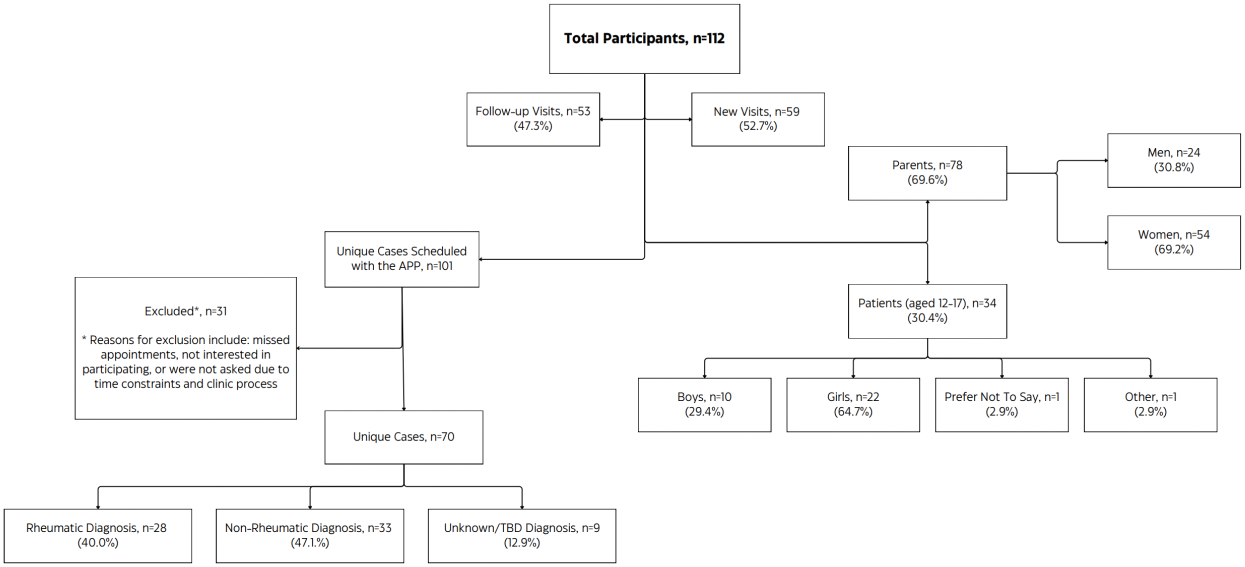
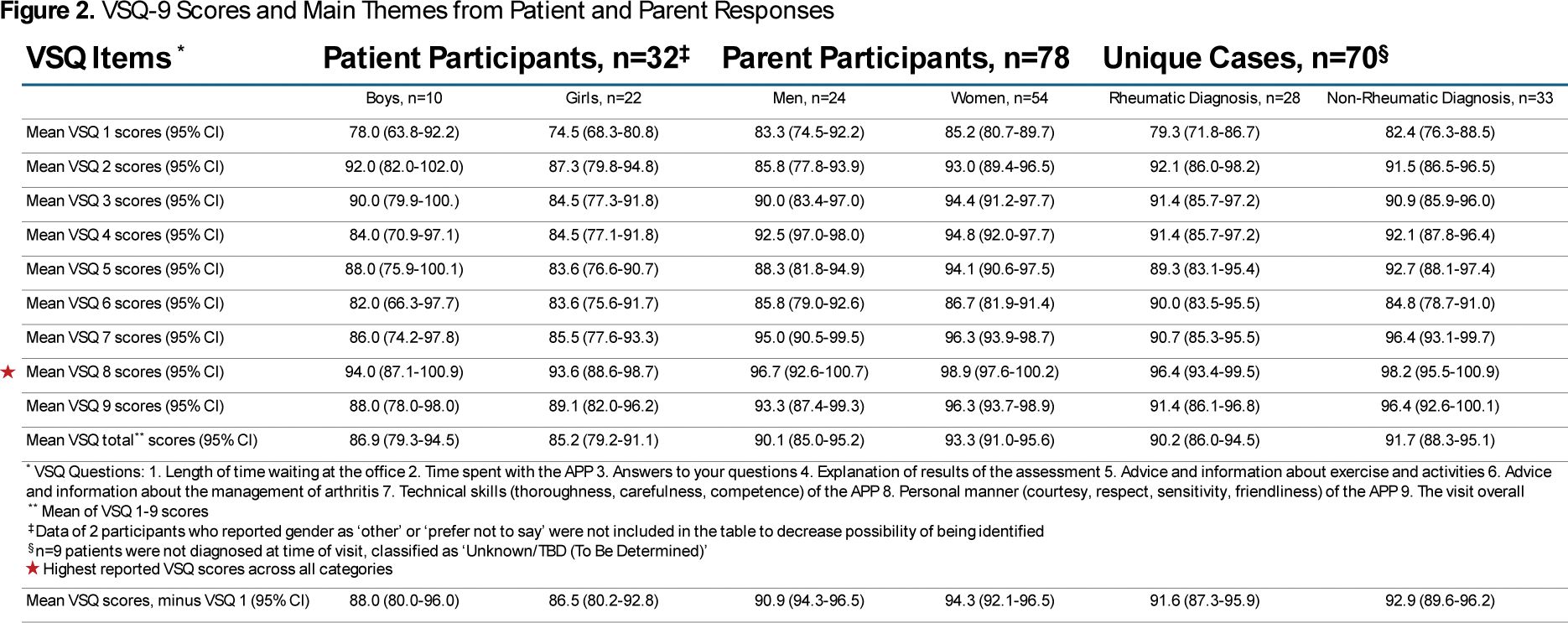
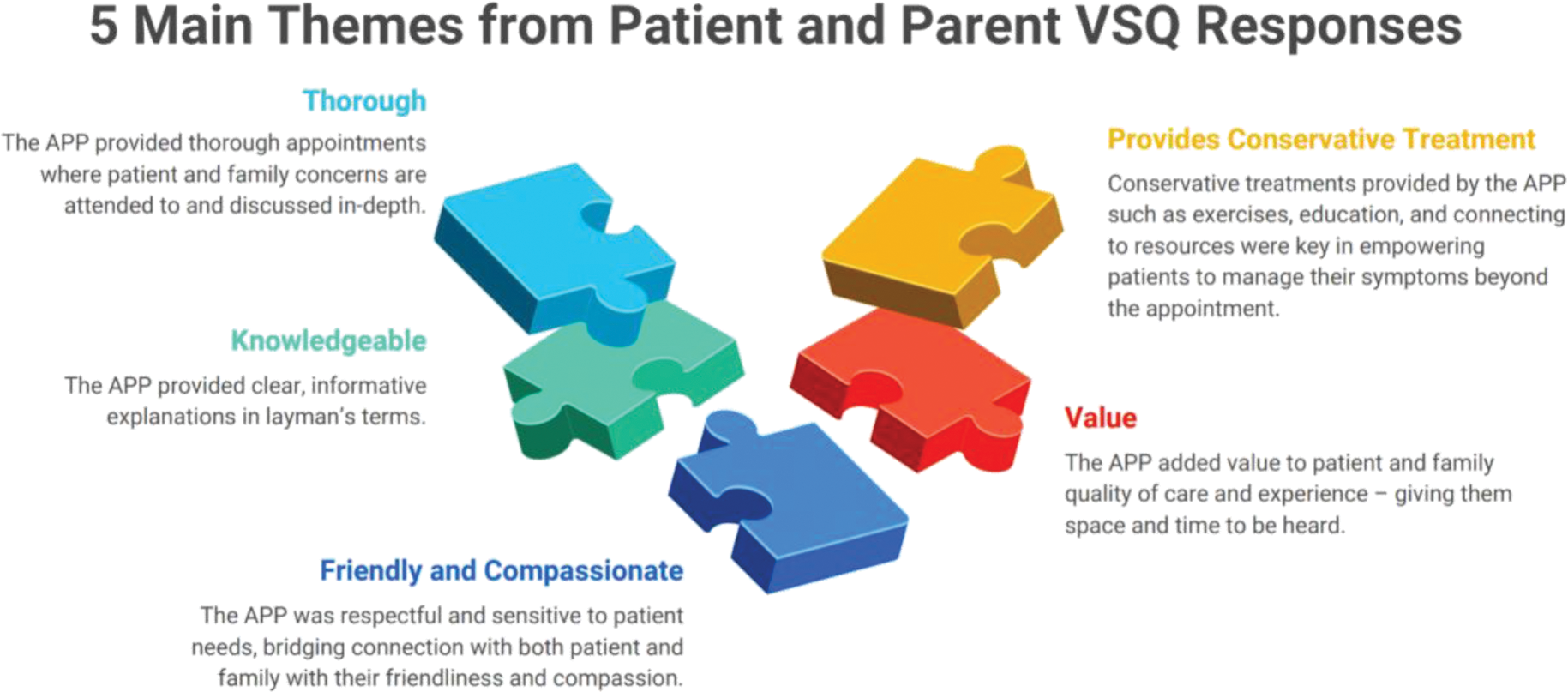
Results: Of 112 participants (n=78 parents, n=34 patients), 53% (n=59) were new consults and 47% (n=53) were follow-ups. Of 101 unique cases scheduled with the APP, 70 consented and were included – 40% (n=28) had a rheumatic disease, 47% (n=33) were non-rheumatic, and 13% (n=9) were considered unknown (Figure 1). Of 78 parents, 69% were women, 46% (n=36) were 41-50 years old, 41% (n=31) travelled >50km to the appointment, and 65% (n=51) held full-time employment. Of 34 patients, 65% (n=22) were girls, 59% (n=20) were Caucasian, mean (SD) age of 15 (1.4) years. Overall visit satisfaction (VSQ9) was high across all participants and conditions, ranging from a mean (95%CI) of 88.0 (78.0–98.0) for boys to 96.3 (93.7–98.9) for women (Figure 2). Overall visit satisfaction (VSQ9) reported by boys and men (88.0 (78.0-98.0), 93.3 (87.4–99.3), respectively) were lower than their counterparts (89.1 (82.0–96.2), 96.3 (93.7–98.9), respectively). Regardless of gender or diagnosis, participants reported the highest satisfaction with the personal manner of the APP (VSQ8). The second highest reporting was time spent with the APP (VSQ2) by patients, and technical skills (VSQ7) by parents. Wait times (VSQ1) had consistently low satisfaction scores. Eliminating VSQ1 (since it is related to clinic process) increased scores by a mean (SD) of 1.1 (0.2). Patient, parent, or APP gender did not appear to impact overall satisfaction with the APP visit. However, two participants (a woman and girl) stated a same-gender APP created a better experience for an adolescent girl, and one man felt APP communication was directed towards the woman parent. Themes from open-ended questions included descriptions of the APP as thorough, knowledgeable, friendly and compassionate, providing conservative treatment, and adding value to their experience.
Conclusion: Overall, participants (parents > patients) reported being highly satisfied with APP shared care model in pediatric rheumatology, consistent with other APP satisfaction literature [4]. Wait times had consistently low satisfaction reporting, previously described as a source of variance in this scale [4]. High reporting of the personal manner of the APP , time spent with the APP, and technical skills of the APP are consistent with the literature [4]. Qualitative themes such as providing a thorough appointment, showing compassion, and bringing value to the patient experience has also been demonstrated in prior APP qualitative studies [4, 5]. These descriptive terms should be considered when explaining an APP shared care model to patients and families. The impact of gender on satisfaction was varied. Women scored the highest satisfaction across all participants. Satisfaction scores of adolescent patients was mixed across gender, but overall lower than parents. To ensure health care delivery meets the expectations of patients and families, next steps include in-depth interviews assessing not only differences in gender but also the different health care needs between adolescents and parents.
REFERENCES: [1] Lundon K. ACR Open Rheumatol. 2020;2(4):242-250.
[2] Thierry S. Joint Bone Spine. 2014;81(2):112-7.
[3] Fennelly O. Musculoskeletal Care. 2018;16:188-208.
[4] OMir M. Pediatr Phys Ther. 2019;31(2):192-199.
[5] Fullerton LM. Pragmat Obs Res 2020;11:1-12.
Acknowledgements: We would like to acknowledge the support of the Canadian Arthritis Health Professions Association for support and mentorship.
Disclosure of Interests: Julie Herrington: None declared, Simran Heera: None declared, Karen Beattie: None declared, Michelle Batthish Educational Grant from NordicPharma 2024.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (