

Background: MAS is a severe complication of rheumatic diseases, most frequently sJIA, caused by excessive activation and expansion of T cells and macrophages. It is characterized by fever, hepatosplenomegaly, liver dysfunction, cytopenias, coagulation abnormalities and hyperferritinemia, possibly progressing to multiple organ failure and death. MAS is categorized as a secondary form of HLH. A vast body of evidence points to uncontrolled overproduction of IFNγ as a major driver of hyperinflammation and hypercytokinemia in MAS and HLH. Emapalumab has been shown to effectively control disease activity in patients with primary HLH.
Objectives: To assess the pharmacokinetics (PK), efficacy and safety of intravenous (IV) emapalumab in patients with MAS and confirm the proposed dose regimen.
Methods: This is a pilot open-label single arm international study (NCT03311854). Patients had to have MAS (defined according to the 2016 ACR/EULAR classification criteria), on a background of confirmed, or high presumption of, sJIA, and inadequate response to high-dose IV glucocorticoids. Emapalumab initial dose was 6 mg/kg and treatment was continued at 3 mg/kg, twice weekly for a total of 4 weeks or less upon achievement of complete response. Serum concentrations of emapalumab, IFNγ-induced chemokine CXCL9 and sIL2R were measured. Safety assessments included adverse events (AEs) and laboratory abnormalities. Efficacy was defined as complete response by week 8, i.e. absence of MAS clinical signs plus white blood cell and platelet counts above lower limit of normal, LDH, AST/ALT<1.5 x upper limit of normal, fibrinogen >100 mg/dL, and ferritin decreased by ≥80% or to <2000 ng/mL, whichever was lower. Twin protocols are in place to recruit 5 patients each in Europe and North America (trial not started yet). We report data on the 6 patients recruited in the European protocol.
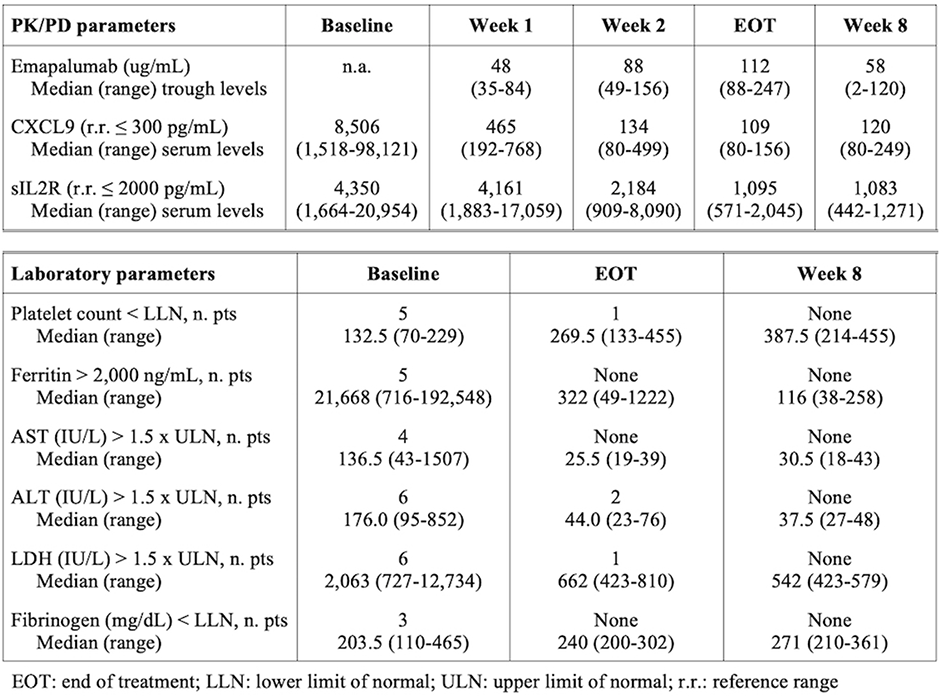
Results: Six patients (5 females, median age 11 years, range: 2-25 years) received emapalumab according to the prescribed dose regimen. Treatment duration ranged from 3 (2 patients) to 4 weeks. Prior to emapalumab, all patients failed methylprednisolone pulses, in 2 patients plus cyclosporine A (CsA) and in 2 patients plus CsA and anakinra. The achieved emapalumab concentrations led to rapid neutralization of IFNγ as indicated by CXCL9 levels and subsequent deactivation of T cells as indicated by sIL2R levels. In all patients, complete response was achieved by week 8, in 4 patients by end of treatment (Table). Systemic glucorticoids were weaned in all patients. Emapalumab infusions were well tolerated and none of the patients discontinued emapalumab. A CMV reactivation was reported by investigator as a serious event possibly related to emapalumab, but resolved completely with treatment.
Conclusion: Emapalumab administration with the tested dosing regimen led to rapid neutralization of IFNγ as shown by normalization of CXCL9, associated with evidence of decreased T cell activation. In all patients, emapalumab treatment was effective in controlling MAS with a favourable safety profile.
REFERENCE:
[1] Ravelli A, et al. Ann Rheum Dis. 2016;75:481-9.
Disclosure of Interests: Fabrizio De Benedetti Grant/research support from: Abbvie, SOBI, Novimmune, Roche, Novartis, Sanofi, Pfizer, Paul Brogan Grant/research support from: SOBI, Novartis, Roche, Novimmune, Chemocentryx, Consultant for: Roche, SOBI, Speakers bureau: SOBI, Roche, Novartis, UCB, Alexei Grom Grant/research support from: Novartis, AB2Bio, Novimmune, Consultant for: Novartis, Pierre Quartier Consultant for: AbbVie, Chugai-Roche, lilly, Novartis, Novimmune, Sanofi, and SOBI, Consultant for: AbbVie, Chugai-Roche, Lilly, Novartis, Novimmune, Sanofi, and SOBI, Speakers bureau: AbbVie, BMS, Chugai-Roche, Novartis, Pfizer, and SOBI, Speakers bureau: AbbVie, BMS, Chugai-Roche, Novartis, Pfizer, and SOBI, Rayfel Schneider Grant/research support from: Roche, Novartis, SOBI, Novimmune, Pfizer, Consultant for: Novimmune, SOBI, Novartis, Kathy De Graaf Consultant for: Novimmune, Employee of: Novimmune, Philippe Jacqmin Consultant for: I am a paid consultant in pharmacology for Novimmune, Maria Ballabio Shareholder of: Novimmune, Employee of: Novimmune, Cristina de Min Shareholder of: Novimmune, Employee of: Novimmune
DOI: 10.1136/annrheumdis-2019-eular.3341