

Background: MSA test is useful to diagnose IIM and subcategorize patients by disease phenotypes.
Objectives: The study aims to evaluate the survival of IIM patients of different MSA patterns.
Methods: An IIM registry had been set up in a tertiary referral centre since 2014 by recruiting prevalent and incident cases. Patients were followed-up prospectively. This study included patients fulfilling the 2017 EULAR/ACR classification criteria for IIM 1 and excluded those aged < 18 at disease onset. Immunoblot EUROLINE autoimmune inflammatory myopathies 16 antigens strip (EUROIMMUNE AG, Lubeck, Germany) was used. Information including baseline demographic data, disease manifestations, MSA results, co-existing malignancy, duration of survival and causes of death were collected. IIM patients were divided into seven groups, which included 1) anti-aminoacyl tRNA synthetase (ARS) 2) anti-MDA5, 3) anti-TIF1γ/anti-NXP2, 4) double positive MSA, 5) other MSAs, 6) negative MSA/MAA (myositis associated antibodies) and 7) positive MAA only. Survival probabilities were compared among different MSA groups by using the Kaplan-Meier method and log-rank test. A two-tailed probability value (p) < 0.05 was considered significant. The study was approved by Kowloon Central Cluster Ethic Committee (ref.: KC/KE-17-0177/ER-3)
Results: Among 112 IIM patients, 79 (70.5%) were female, and the median age of onset was 55 (18-90) years old; 63.4% were dermatomyositis (DM), 17.9% polymyositis (PM) and 18.8% clinically amyotrophic DM (CADM). Co-existing interstitial lung disease (ILD) was common and found in 65 (58%) patients; 16 (14.3%) had rapidly progressive interstitial lung disease (RPILD), and 16 (14.3%) died within the observed period. Overall, the commonest cause of death was RPILD, followed by infection and malignancy. While anti-MDA5 was strongly associated with RPILD (odds ratio = 33.0 [95% CI: 7.2-151.8], p<0.001), anti-MDA5 group had the worst survival, with 1-year and 5-year survival both at 43%, compared to above 80% in all other groups (log-rank test p<0.001) (
Conclusion: Anti-MDA5 associated RPILD was the leading cause of mortality in IIM. However, those tested negative for both MSA and MAA by current immunoblot technique also had guarded prognosis related to the risk of infection and malignancy.
Kaplan-Meier survival of IIM
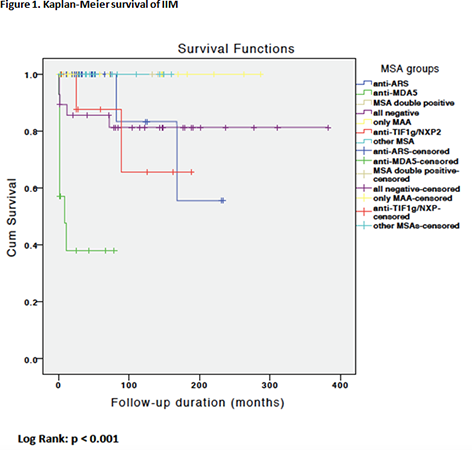
Survival rates in different MSA groups
| Survival | 1 year | 5 years |
| Anti-ARS | 100% | 92% |
| Anti-MDA5 | 43% | 43% |
| Double positive | 100% | 100% |
| Negative MSA/MAA | 89% | 82% |
| Only positive MAA | 100% | 100% |
| Anti-TIF1γ/anti-NXP2 | 100% | 88% |
| Other MSAs | 100% | 100% |
REFERENCES:
[1] Lundberg IE, et al.. ARD2017;76(12):1955-1964.
Disclosure of Interests: None declared
DOI: 10.1136/annrheumdis-2019-eular.3185