

Background: Hydroxychloroquine (HCQ) has been used safely for over 60 years in rheumatic patients. However, following its recent use in covid-19 disease, its safety has been questioned, following controversial reports of cardiac toxicity 1 , possibly related to a prolongation of the QT interval 2 .
Objectives: To explore the influence of chronic treatment with hydroxychloroquine on QT interval in rheumatic patients, and the possible effects of drug-to-drug interference 3 .
Methods: 12-lead electrocardiogram tracings were recorded with standard equipment in 229 ambulatory patients (SLE = 53, RA = 52, SSc = 56, UCTD = 38, Others = 30). The present analysis was performed on corrected QT intervals (QTc) calculated according to Framingham formula (QTc = QT+0.154 (1−RR)), with ULN = 449 ms in males, and 467 ms in females. Estimated glomerular filtrate rate (eGFR) was calculated from serum creatinine with the CKD-EPI equation. The influence on QTc values of demographic variables, chronic (≥3 months) HCQ treatment, and of the use of selected comedications -Statins, Angiotensin Converting Enzyme inhibitors (ACEi), Angiotensin Receptor Blockers (ARBs), Selective Serotonin Reuptake Inhibitors (SSRIs), Proton-Pump Inhibitors (PPI), Calcium Channel Blockers (CCBs) – were evaluated by parametric or non parametric statistical methods, as appropriate. All statistic al analyses were performed with the IBM SPSS statistical package version 25.
Demographic and clinical variables in patients treated with HCQ (HCQ+) and in controls (HCQ-).
| N | Age
| Female
| eGFR
| Statins
| ACEi
| ARB
| SSRI
| PPI
| CCB
|
|
| All | 229 | 58.02
| 206
| 87.14
| 29
| 48
| 19
| 14
| 138
| 30
|
| HCQ+ | 132 | 58.71
| 122
| 87.00
| 18
| 32
| 11
| 9
| 80
| 17
|
| HCQ- | 97 | 57.51
| 84
| 87.32
| 11
| 16
| 8
| 5
| 58
| 13
|
| p | 0.532 | 0.183 | 0.897 | 0.690 | 0.189 | 1.000 | 0.782 | 1.000 | 1.000 |
Demographic variables, and the use of evaluated comedications were not different in HCQ+ and HCQ- patients (
QTc duration was not associated with the use of Statins, ACEi, ARBs, or SSRIs (p = 0.454, 0.276, 0.475, and 0.131 respectively), but was significantly prolonged in patients treated with HCQ (421.26 ± 19.19 vs 410.55 ± 21.18 msec, p < 0.001), PPIs (420.57 ± 21.45 vs 410.89 ± 18.12 ms, p < 0.001), and CCBs (424.22 ± 25.97 vs 415.59 ± 19.62 ms, p < 0.033). Furthermore, as reported in
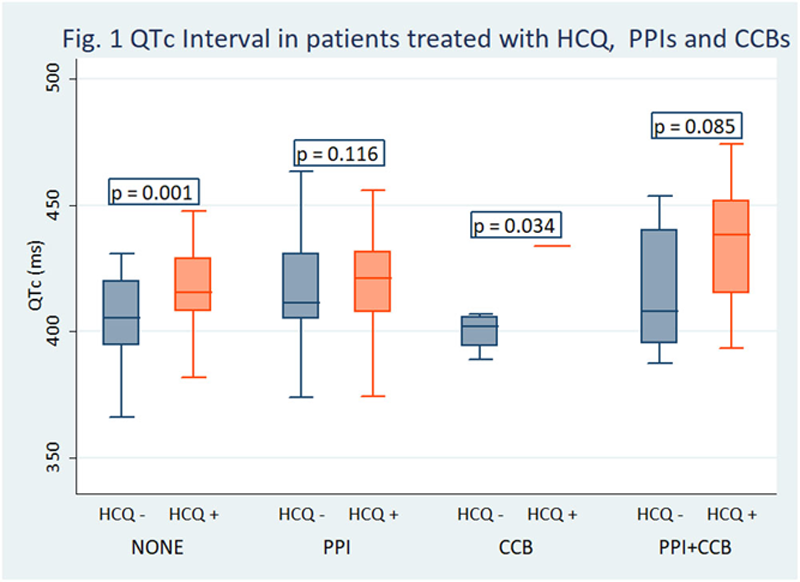
Conclusion: In this study, the QTc interval was significantly prolonged in patients treated with hydroxychloroquine as compared to controls, although significant prolongation was extremely infrequent. Furthermore, our data revealed signs of drug-drug interference, suggesting that regular monitoring of the electrocardiogram is advisable in these patients, often undergoing cotreatment with multiple drugs.
REFERENCES:
[1]Imad M. Tleyjeh, et al. The Cardiac Toxicity of Chloroquine or Hydroxychloroquine in COVID-19 Patients: A Systematic Review and Meta-regression Analysis. Mayo Clin Proc Innov Qual Outcomes. 2020 Nov 2 doi: 10.1016/j.mayocpiqo.2020.10.005 [Epub ahead of print].
[2]Teodoro J. Oscanoa, et al. Frequency of Long QT in Patients with SARS-CoV-2 Infection Treated with Hydroxychloroquine: A Meta-analysis. Int J Antimicrob Agents.
[3]Byung Jin Choi, et al. Risk of QT prolongation through Drug-drug Interactions between Hydroxychloroquine and Concomitant Drugs Prescribed in Real-world Practice. Preprint from Research Square, 22 Sep 2020 DOI: 10.21203/rs.3.rs-79572/v1 PPR: PPR217328.
Disclosure of Interests: None declared