

Background: Systemic lupus erythematosus (SLE), a multisystem autoimmune disease, is associated with mental health (MH) disorders. There is scarce information on the epidemiology and economic burden associated with MH comorbidities and the impact on SLE as well as the subpopulation with lupus nephritis (LN).
Objectives: Examined the incidence and prevalence rate of MH, healthcare resource utilization (HCRU), and costs associated with MH comorbidities in SLE/LN patients.
Methods: Adult SLE and LN patients with ≥1 inpatient or ≥2 outpatient diagnosis claims for SLE/LN (ICD-9 code: 710.0; and ICD-10 codes M32.10-19, M32.8, M32.9) were identified between 01JAN2013-30JUN2019 from two large US commercial databases. Inclusion required continuous enrollment benefits 12 months pre-/post-index date. Patients were divided into two groups: those with (WMH) vs. those without (NMH). WMH was defined as a MH diagnosis of depression, anxiety, bipolar disorder, or psychosis. Index date for the WMH group was first MH diagnosis claim. For the NMH group, a random index date was assigned between 01JAN2014-30JUN2018. The groups were then matched with a 1:1 ratio based on age, sex, and region within their respective databases. Incidence and prevalence rate of MH in the SLE/LN population were determined. All-cause healthcare costs and HCRU per patients per year (PPPY) were examined with generalized linear models.
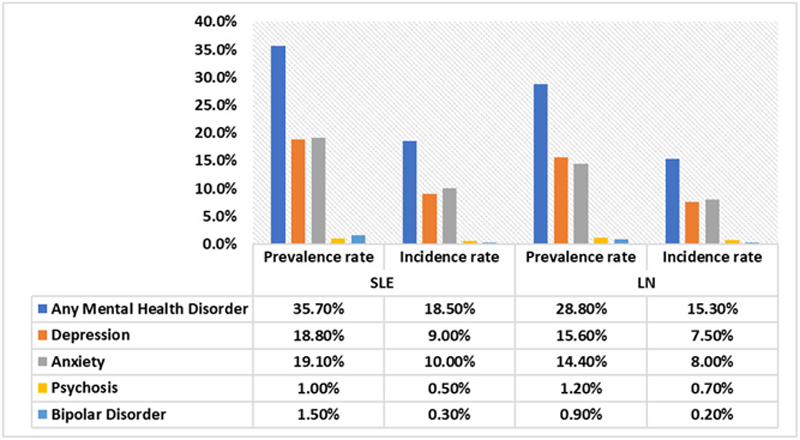
Results: A total of 7,760 SLE and 336 LN patients were identified. The majority of patients were female (SLE=93.5%; LN=95.2%) with a mean age of 55.1 years (SLE) and 44.5 years (LN). The prevalence rate of MH was 35.7% for SLE and 28.8% for LN patients and the incidence rate was 18.5% and 15.3%, respectively. Anxiety and depression were the most common MH comorbidities (
Follow-up Healthcare Cost and Utilization for SLE/LN Case and Control Population
| SLE with MH Comorbidities N=3,880 (WMH) | SLE without MH comorbidities N=3,880 (NMH) | P-value | LN with MH Comorbidities N=168 (WMH) | LN without MH comorbidities N=168 (NMH) | P-value | |
| All-cause health care utilization PPPY | Mean | Mean | Mean | Mean | ||
| Mean # inpatient visits | 1.36 | 0.50 | <0.0001 | 1.86 | 0.86 | <0.0001 |
| Mean # outpatient visits | 32.11 | 21.67 | <0.0001 | 47.85 | 29.45 | <0.0001 |
| Mean # office visits | 13.49 | 9.74 | <0.0001 | 14.94 | 10.29 | <0.0001 |
| Mean # ER visits | 1.27 | 0.66 | <0.0001 | 1.40 | 0.63 | 0.0005 |
| Mean # other outpatient visits | 25.55 | 17.08 | <0.0001 | 41.48 | 24.19 | <0.0001 |
| Mean # pharmacy Rx | 33.33 | 20.82 | <0.0001 | 36.96 | 23.81 | <0.0001 |
| Length of inpatient stay (mean, days) | 3.69 | 1.09 | <0.0001 | 9.53 | 2.37 | <0.0001 |
| All-cause health care costs PPPY | ||||||
| Outpatient costs (ER+ office +other) | $19,271 | $12,847 | <0.0001 | $34,956 | $19,530 | <0.0001 |
| Pharmacy costs | $7,222 | $4,707 | <0.0001 | $7,874 | $4,254 | <0.0001 |
| Inpatient costs | $22,605 | $8,191 | <0.0001 | $68,216 | $14,680 | <0.0001 |
| Total costs | $49,553 | $26,064 | <0.0001 | $112,169 | $39,529 | <0.0001 |
PPPY: Per patient per year; ER: Emergency room; LN: Lupus nephritis; SLE: Systemic lupus erythematosus
Conclusion: This real-world study shows that MH comorbidities have a high incidence and prevalence rate in SLE and LN patients. Health care costs and utilization for SLE and LN patients with MH comorbidities were significantly higher than patients without MH comorbidities. This study highlights not just the high prevalence of MH comorbidity but its large contribution to SLE healthcare costs.
Incidence and Prevalence Rate of Mental Health Comorbidities in the SLE and LN Populations LN: Lupus nephritis; SLE: Systemic lupus erythematosus
Disclosure of Interests: Michelle A Petri Consultant of: Yes, Grant/research support from: Yes, Dominik Naessens Shareholder of: Yes (Johnson and Johnson), Employee of: Employee of Janssen Pharmaceuticals., Adesuwa Ogbomo: None declared, Anna Ratiu: None declared, Cynthia Gutierrez: None declared, Chetan Karyekar Shareholder of: Own Stock Options as part of being a company employee., Employee of: Current employee of Janssen Pharmaceuticals