

Background: Microscopic polyangiitis (MPA) is an anti-neutrophil antibody (ANCA)-associated vasculitis(AAV) predominantly affecting small vessels and organs, such as the skin, lung, heart, and kidney. Although some studies have used cluster analysis to identify the clinical phenotype of AAV, no study to date has focused on the clinical phenotype of MPA[1, 2]. It has not been elucidated whether differences in clinical background determine prognosis in MPA, so the stratification of patients based on their clinical background is crucial for improving the prognosis of MPA.
Objectives: This study aimed to identify new clinical phenotypes of MPA using a principal components analysis (PCA)-based cluster analysis.
Methods: A total of 189 patients with MPA between May 2005 and December 2021 were enrolled from a multicenter cohort in Japan (REVEAL cohort). Categorical PCA and cluster analysis were performed based on clinical, laboratory, and radiological findings. Clinical characteristics and outcomes, including all-cause mortality, respiratory-related mortality, end-stage renal disease (ESRD), and relapse were compared between each cluster.
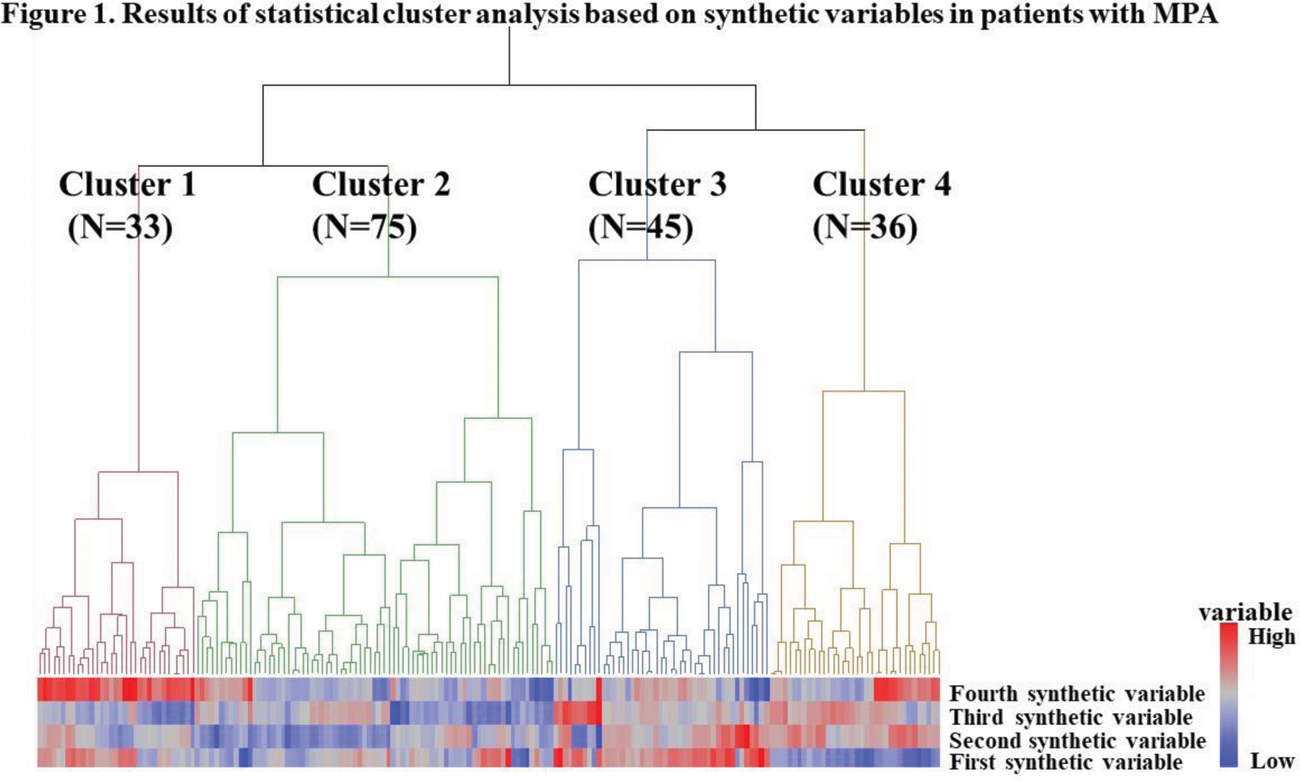
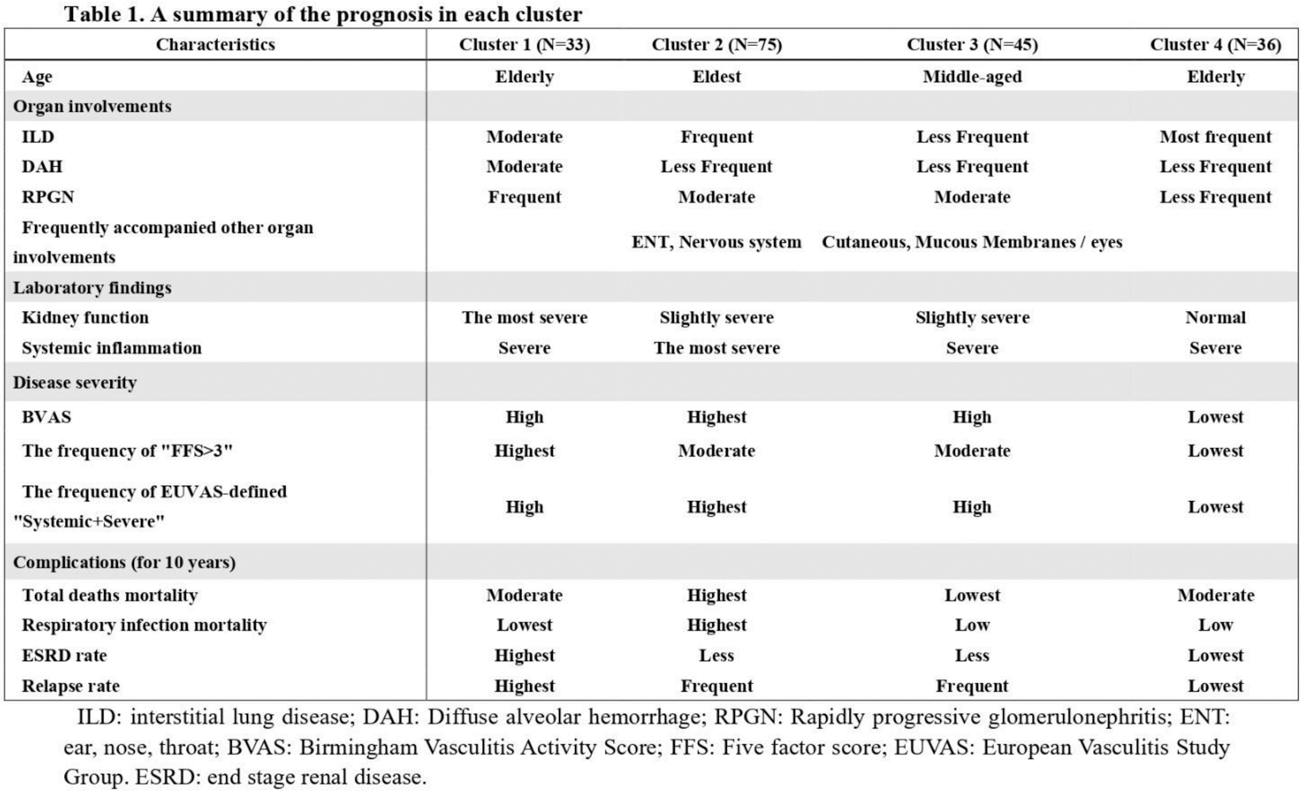
Results: Eleven clinical variables were transformed into four components using categorical PCA and synthetic variables were created. Additionally, a cluster analysis was performed using these variables to classify patients with MPA into subgroups (shown in Figure 1). Four distinct clinical subgroups were identified: Cluster 1 included the renal involvements and diffuse alveolar haemorrhage (DAH)-dominant group (N=33). Cluster 2 comprised the elderly onset systemic inflammation group (N=75). Cluster 3 included patients in the younger-onset limited-organ disease group (N=45). Cluster 4 was comprised of an ILD-predominant group without kidney involvement (N=36). 61 patients died during follow-up, with 32 dying of respiratory-related causes. Additionally, 19 patients developed ESRD and 70 relapsed. Cluster 1 showed the worst ESRD-free survival and relapse rates, whereas Cluster 2 showed the worst overall survival and respiratory-related death-free survival rates among the four groups (shown in Table 1).
Conclusion: Our study identified four unique subgroups with different MPA outcomes. Individualized treatments for each subgroup may be required to improve the prognosis of MPA.
REFERENCES: [1] Mahr A, Katsahian S, Varet H, et al. Revisiting the classification of clinical phenotypes of anti-neutrophil cytoplasmic antibody-associated vasculitis: a cluster analysis. Ann Rheum Dis 2013;72(6):1003-10.
[2] Watanabe H, Sada KE, Harigai M, et al. Exploratory classification of clinical phenotypes in Japanese patients with antineutrophil cytoplasmic antibody-associated vasculitis using cluster analysis. Sci Rep 2021;11(1):5223.
Acknowledgements: NIL.
Disclosure of Interests: Ayana Okazaki: None declared, Shogo Matsuda Speakers bureau: Abbvie, Grant/research support from: Japan Intractable Diseases Research Foundation, Takaho Gon: None declared, Ryu Watanabe Speakers bureau: Asahi Kasei, Eli Lilly, Chugai, GlaxoSmithKline, Sanofi, Grant/research support from: AbbVie, Atsushi Manabe: None declared, Mikihito Shoji: None declared, Keiichiro Kadoba: None declared, Wataru Yamamoto: None declared, Ryosuke Hiwa Speakers bureau: Daiichi Sankyo, Takuya Kotani Speakers bureau: AbbVie, Bristol-Myers Squibb, Chugai, Eisai, Eli Lilly, Pfizer, Motomu Hashimoto Speakers bureau: Eli Lilly, Chugai, Tanabe-Mitsubishi, Bristol-Myers Squibb, Esai, Grant/research support from: AbbVie, Asahi Kasei, Astellas, Bristol-Myers Squibb, Esai, Daiichi Sankyo, Eli Lilly, Novartis, Tohru Takeuchi Speakers bureau: Asahi Kasei, Chugai, Bristol-Myers Squibb, Tanabe-Mitsubishi, AbbVie, Esai, Grant/research support from: Chugai.