

Background: Anti-melanoma differentiation association protein 5 autoantibodies (anti-MDA5) are associated with interstitial lung disease (ILD), particularly with rapidly progressive ILD (RP-ILD) amongst Asian patients with amyopathic dermatomyositis (ADM). Both high anti-MDA5 and serum ferritin levels have been suggested as a poor prognostic marker in anti-MDA5+ RP-ILD, and anti-MDA5 levels to potentially correlate with disease activity longitudinally. These reports are mainly from Asian cohorts, who may have a more severe disease phenotype, and little is known if this can be applied to Caucasian cohorts.
Objectives: This study aims to determine whether longitudinal anti-MDA5 levels correlate with laboratory and clinical markers of disease activity in a Swedish cohort of patients with anti-MDA5+ dermatomyositis (DM).
Methods: Serum samples (n=54) from 16 patients with DM (of which two with ADM according to EULAR/ACR classification criteria) were collected longitudinally at Karolinska University Hospital between 1999 and 2021. All patients were positive for anti-MDA5 tested by ELISA, Line Blot or Immunoprecipitation. An in-house ELISA was developed to screen retrospectively the longitudinal serum samples for antibody levels against a recombinant full-length MDA5 protein (cut off 1.07µg/mL). Commercial assays were used to retrospectively measure ferritin (mikrogr/L), creatine kinase (CK, mikrokat/L), C-reactive protein (CRP, mg/L), and lactate dehydrogenase (LD, mikrokat/L) levels. Prospectively collected clinical data from the same time of sampling, including pulmonary function test variables (diffusing capacity for carbon monoxide (DLCO) and forced vital capacity (FVC) expressed in % of predicted values) was retrieved retrospectively. Remission and low disease activity was defined by physician global assessment (PhGA) ≤20 and/or physician’s judgement. Variables were presented as medians with inter-quartile range (IQR). Wilcoxon, Mann-Whitney and Spearman’s correlation tests were conducted.
Results: In total, 54 samples, ranging from 2 to 5 samples per patient, were analysed. Median duration between diagnosis and baseline sample was 0 months (ranging from 2 months prior to 35 months after diagnosis), while median time interval between diagnosis and last sample was 38.5 months (ranging from 7 months to 214 months). Majority of patients (12/16) had ILD but only two patients developed RP-ILD. All patients, except for one from Asia with non-RP-ILD, were Caucasians. At time of baseline sampling, patients presented with moderate-high disease activity with a median PhGA of 60 (IQR 20) correlating only with CK (median 0.3 (0.4), r=0.71, p=0.02). When analysing instead the pooled 54 samples, PhGA correlated with anti-MDA5 (r=0.68, p< 0.0001), ferritin (r=0.4, p=0.004), and LD (r=0.4, p=0.002) levels, but not with CK. We observed, at baseline, a tendency towards higher median levels of anti-MDA5 and ferritin (269.9 (286.4), 1115 (1244.5), respectively) in the ILD group compared to patients without ILD (74.7 (440.7), 434 (1279), respectively). In eight patients (one without ILD) with available spirometry data at matching sampling time points, baseline anti-MDA5 levels were inversely correlated with FVC% (median FVC 68% (30), r -0.9, p=0.005) and DLCO% (median DLCO 62% (20), r= -0.8, p=0.02). This was also confirmed in the pooled samples, as anti-MDA5 levels correlated with FVC and DLCO (paired 22 and 18, respectively). Moreover, at follow-up samples, a longitudinal reduction in anti-MDA5 levels was associated with recorded improved/stabilized lung disease activity by the responsible physician in all 12 patients at corresponding sampling times. The pooled anti-MDA5 levels were moderately correlated with the pooled ferritin (r 0.44, p=0.001) and CRP levels (r=0.33, p=0.02). In the entire cohort, baseline median anti-MDA5 (227 (319.8)) levels were higher than last sample levels (1.87 (5.21) p<0.0001), as well as baseline ferritin (1026 (1343)) compared with last ferritin (163 (89), p=0,01). There was also significant reduction from baseline PhGA (60 (20) to last PhGA (10 (15), p=0.001). At first follow up sample, 6/16 patients had anti-MDA5 levels under cut-off, of which 5 were either in remission or low disease activity and one patient was in a current flare but had received rituximab (1000 mg x 3) during the 5 months prior to sampling. Only one patient had a noticeable increase of anti-MDA5 levels (+42.12) with increased ferritin (+358) and PhGA (+22) at corresponding time point (Figures 1 and 2).
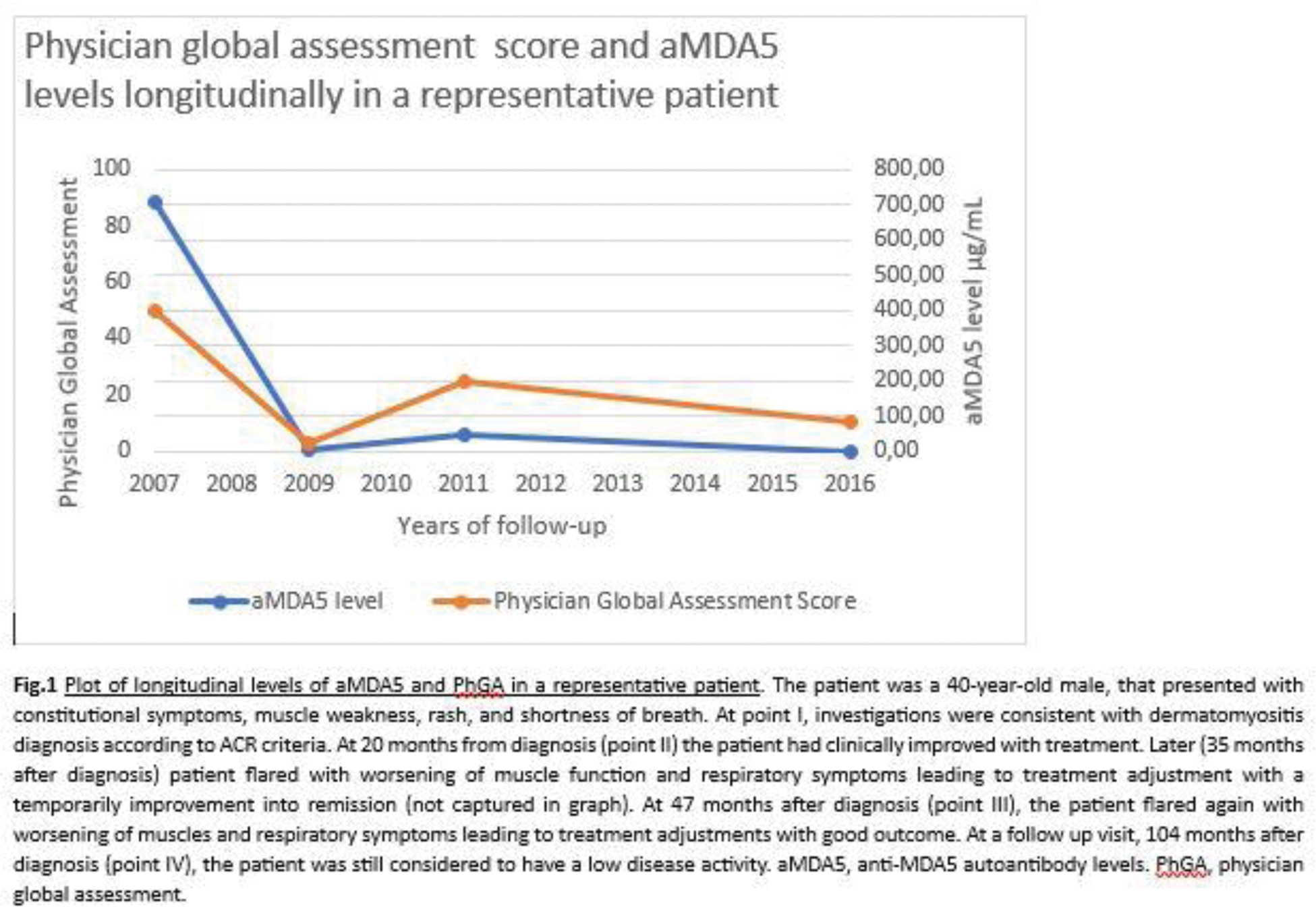
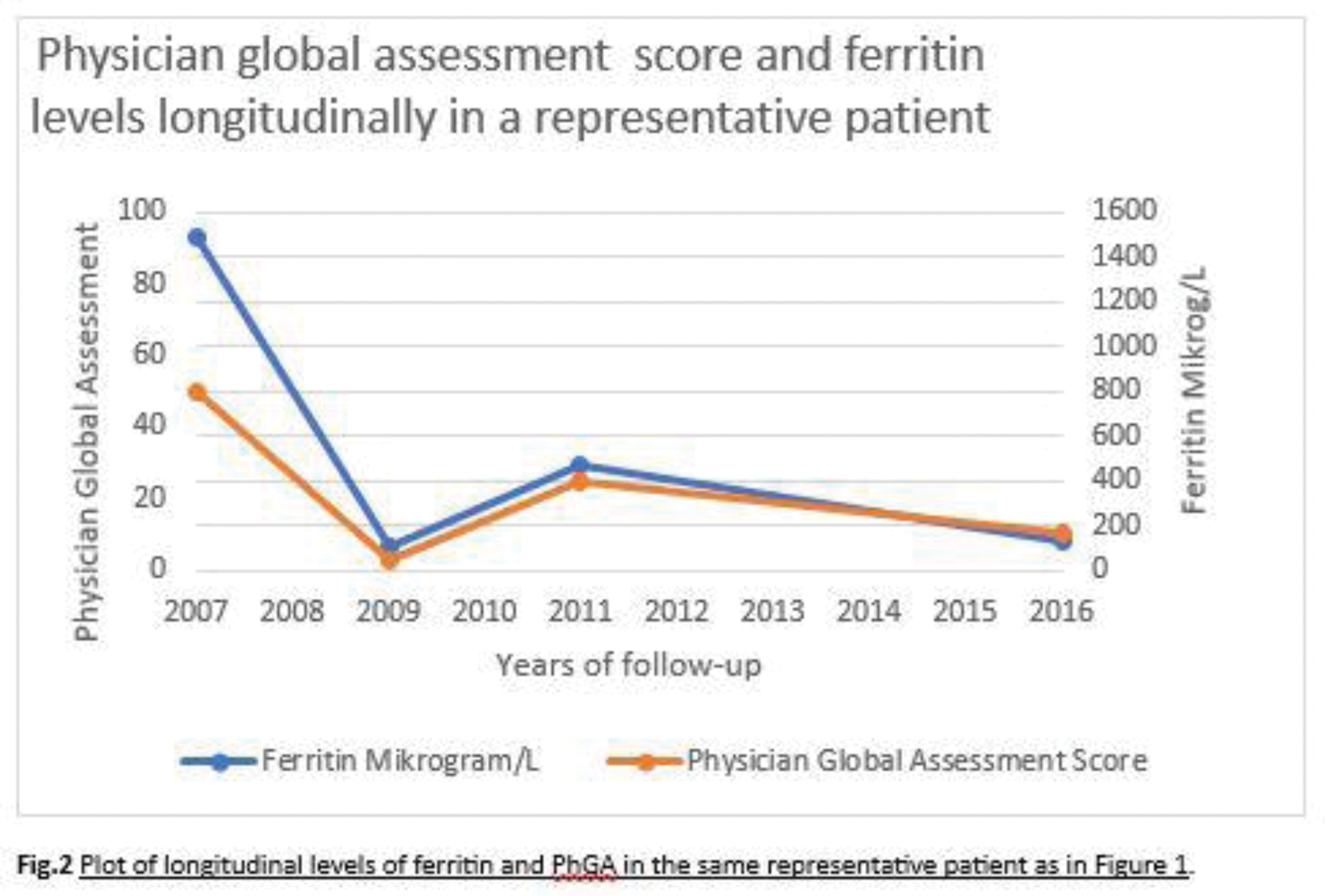
Conclusion: Our results suggest that both anti-MDA5 and ferritin may be used as biomarkers for monitoring disease activity in Caucasian patients with anti-MDA5 positive DM. Interestingly, only longitudinal changes in anti-MDA5 levels correlated with pulmonary function tests and lung progression over time. Further studies including longitudinal data are required to confirm our preliminary findings in Caucasian cohorts of anti-MDA5 positive DM.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (