

Background: Optic Neuritis is both a rare manifestation of Systemic Lupus Erythematosus (SLE) and a prominent feature of Neuromyelitis Optica Spectrum Disease (NMOSD), involving immune-mediated inflammation in the central nervous system (CNS) that leads to demyelination and vision loss. The overlapping neurological features of SLE and NMOSD complicate diagnosis and demand distinct treatment approach, especially in refractory cases.
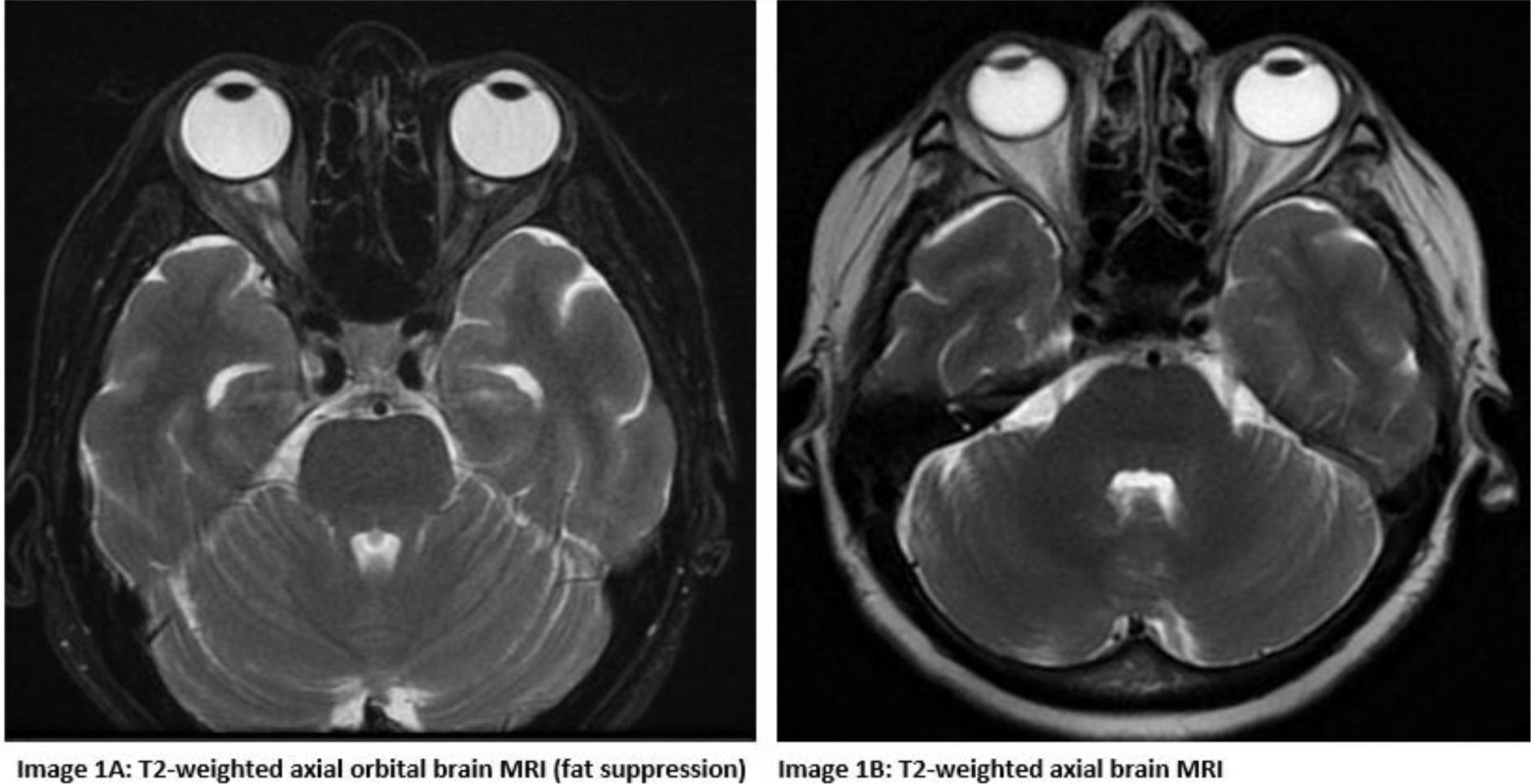
Case presentation: A 64-year-old female with arterial hypertension and mild thrombocytopenia presented with progressive vision loss over 2 months. Clinical examination was normal. Ophthalmologic assessment showed severe visual impairment: light perception in the right eye and finger counting at 2 meters in the left, without signs of inflammation or macular edema. Brain CT and CTA scans were unremarkable. Laboratory results confirmed mild thrombocytopenia (PLT: 80×10^3), normal inflammatory markers, urinalysis and biochemical panel. Brain MRI revealed mild enhancement of the right optic nerve, indicating optic neuritis. (Image 1A) Cerebrospinal fluid analysis was normal. Serological tests showed elevated anti-aquaporin-4 antibodies (32× ULN), hypocomplementemia (C3: 73.7 mg/dL; C4: 10 mg/dL), and high anti-dsDNA binding (2× ULN), confirming coexistent NMOSD and SLE. Treatment with steroids and Rituximab (RTX) led to mild visual improvement (left eye: 8/10; right eye: 2/10) and normalization of platelets (PLT: 326×10^3). Maintenance therapy with RTX and Azathioprine prevented relapses over a two-year follow-up period and MRI showed right optic nerve atrophy without new lesions. (Image 1B)
Learning points for clinical practice: Optic neuritis in NMOSD is associated with systemic autoimmune disorders like SLE and can present with transverse myelitis. NMOSD is typically linked to antibodies against Aquaporin-4 (AQP-4) or Myelin-Oligodendrocyte-Glycoprotein (MOG) and lacks systemic involvement, unlike SLE. While both conditions require high-dose steroids and immunosuppressants, treatment may differ. NMOSD first-line treatments include biologics such as Eculizumab (anti-C5a), Inebilizumab (anti-CD19), Satralizumab (anti-IL-6) and plasma exchange [1]. In contrast, CNS Lupus is treated with cyclophosphamide and RTX for refractory cases. This case underscores the complex coexistence of NMOSD and SLE, highlighting the diagnostic challenges posed by overlapping autoimmune disorders. Optic neuritis, while prominent in NMOSD, is rare in SLE, potentially delaying diagnosis and treatment. Early recognition and targeted therapy of the dominant disease are vital to preventing irreversible damage and improving outcomes, emphasizing the need for further research into these intersecting conditions.
REFERENCES: [1] Ochi MGS et al.Lupus and NMOSD: The Blending of Humoral Autoimmunity. Case Rep Rheumatol.2020 Oct15;2020:8820071.
Acknowledgements: Consent for publication obtained directly from patient.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (