

Background: Relapsing polychondritis (RP) is a rare disorder characterized by recurrent inflammation of cartilaginous tissues throughout the body. Airway cartilage involvement can result in severe complications such as respiratory failure, posing a significant threat to patient survival. Effective treatment strategies are urgently needed. Current standard therapies, including glucocorticoids (GC) and immunosuppressants, often fail to manage refractory RP, making it particularly challenging to achieve steroid-free management. Recently, the efficacy of biologic agents such as tumor necrosis factor-alpha (TNFα) inhibitors and interleukin-6 (IL-6) inhibitors in RP has been reported. However, due to the rarity of RP, robust evidence from large-scale prospective studies or randomized controlled trials remains limited, and long-term outcomes are not well-established. At our institution, a specialized RP clinic receives numerous referrals for refractory RP cases from across Japan.
Objectives: To evaluate the long-term efficacy of biologic agents in the treatment of refractory RP.
Methods: A retrospective cohort study was conducted on patients diagnosed with RP based on McAdam’s criteria, who visited St. Marianna University School of Medicine between April 1, 2005, and March 31, 2024. Disease activity was assessed using the Relapsing Polychondritis Disease Activity Index (RPDAI). Treatment effectiveness was defined as improvement in the Visual Activity Scale (VAS) and the ability to taper GC. Data collection included patient demographics, clinical symptoms, laboratory findings, treatment regimens, disease activity, and adverse events. Biologic agents (TNFα inhibitors, IL-6 inhibitors, CD20 inhibitors) were analyzed for their effects on RPDAI, symptom-specific VAS improvement, GC tapering, and continuation rates. Factors influencing continuation rates were also analyzed. Statistical analyses included the Mann-Whitney U test for continuous variables and Fisher’s exact test for categorical variables. Kaplan-Meier analysis was used to evaluate continuation rates.
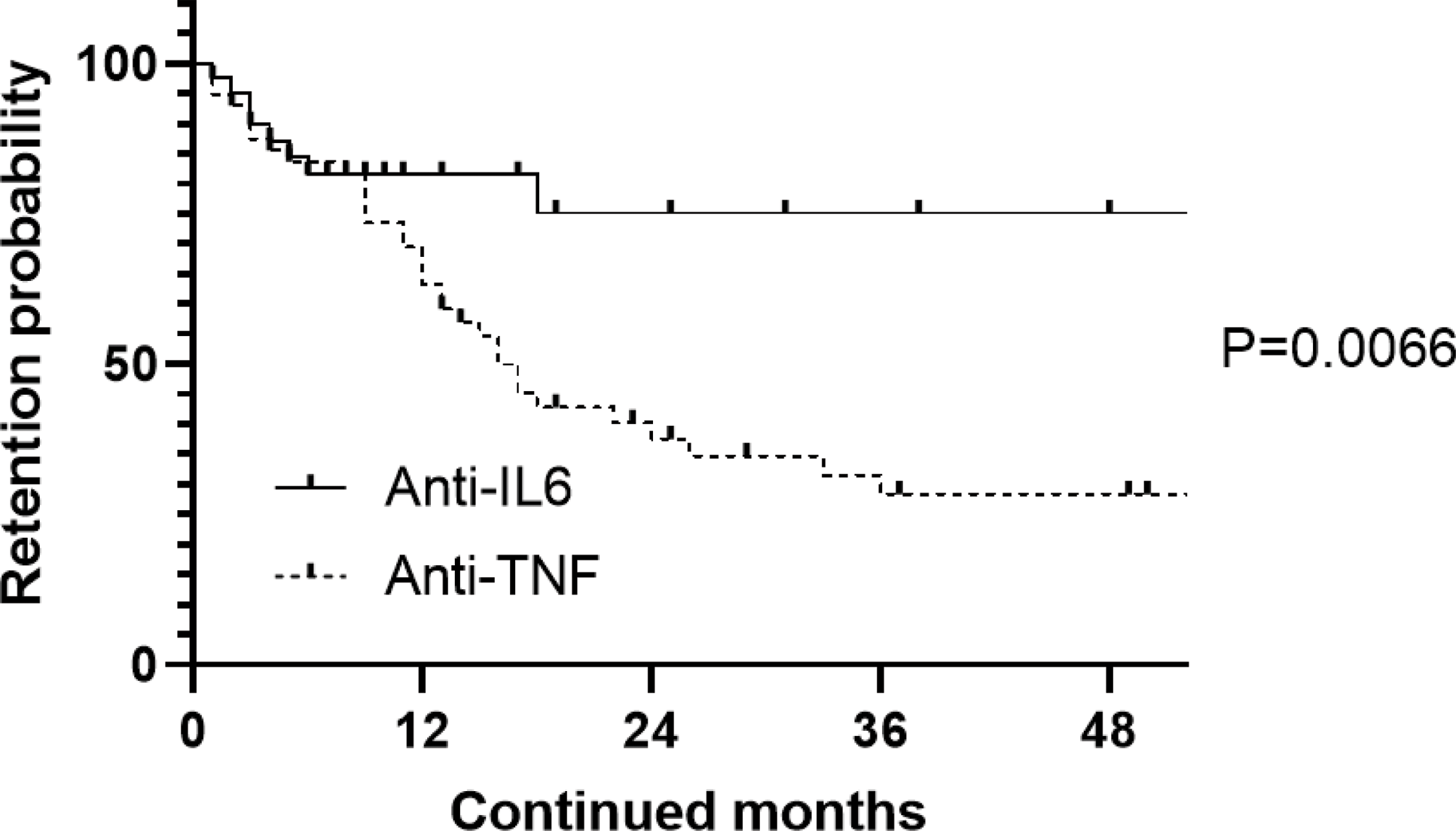
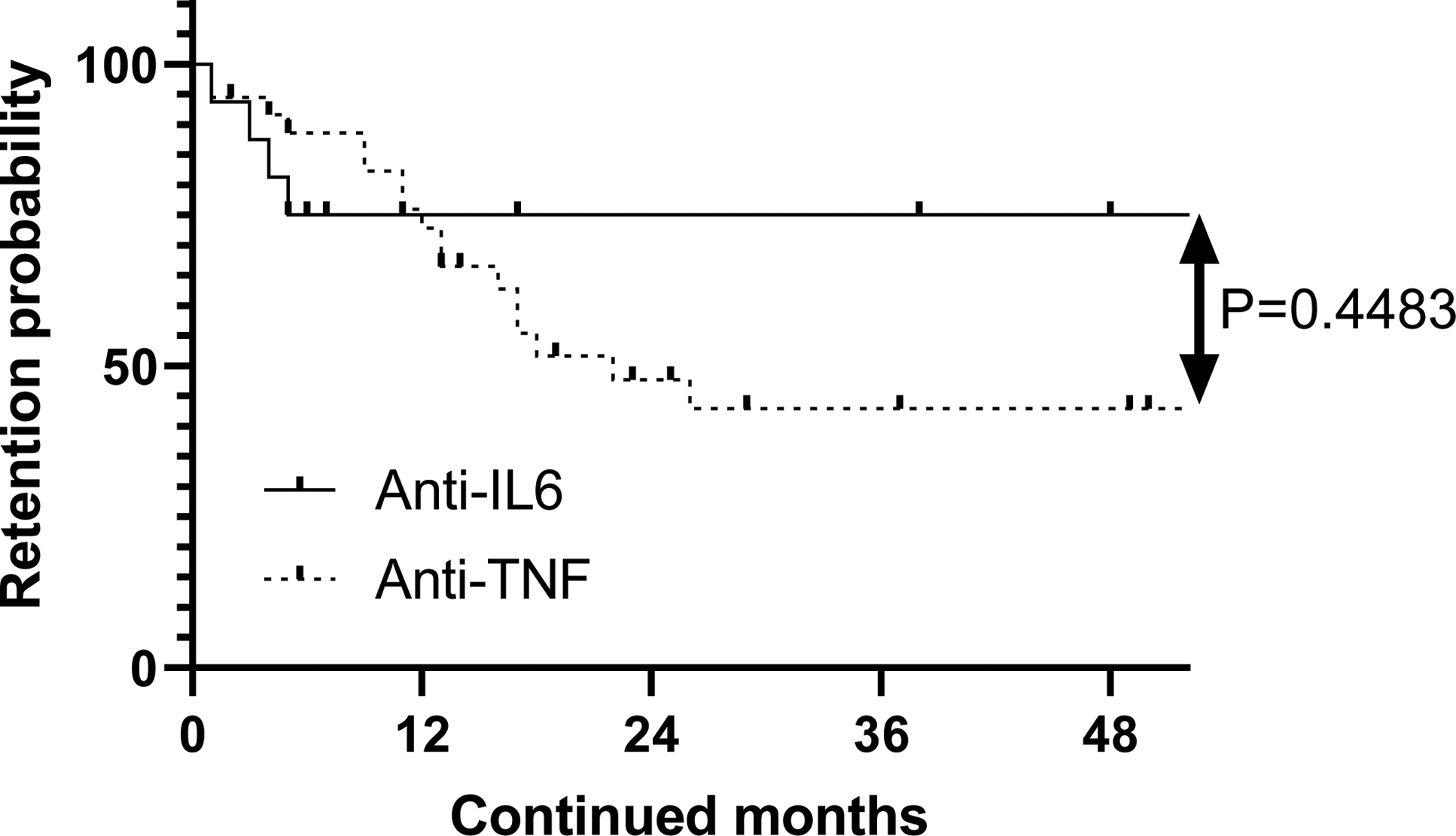
Results: Among 183 RP patients, 110 required immunosuppressive therapy. Biologic agents were used in 62 refractory cases, with a mean age of 48 years, 56.5% female, and 44 cases (71.0%) presenting with airway involvement. TNFα inhibitors were used in 44 of 70 patients (62.9%), IL-6 inhibitors in 42 of 53 patients (79.3%), and CD20 inhibitors in 4 patients, all showing efficacy. Continuation rates were significantly higher for IL-6 inhibitors than for TNFα inhibitors (p=0.006, Figure 1). However, within the first year, dropout rates were higher for IL-6 inhibitors than for TNFα inhibitors (Figure 2). These findings suggest that IL-6 inhibitors are essential for long-term maintenance therapy, while TNFα inhibitors are more effective in the induction phase. Approximately 46% of patients achieved GC-free status during long-term follow-up, with 7 patients (10.0%) in the TNFα inhibitor group, 19 patients (35.8%) in the IL-6 inhibitor group, and 1 patient in the CD20 inhibitor group. The mean time to achieve GC-free status was 581.5 days.
Conclusion: The two-phase treatment strategy of induction therapy with TNFα inhibitors followed by maintenance therapy with IL-6 inhibitors appears effective for managing refractory RP. This approach has the potential to achieve steroid-free management in a significant proportion of patients.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (