

Background: Adult-onset Still’s disease (AOSD) is a rare systemic inflammatory disorder of unknown etiology, characterized by arthritis, fever and maculopapular rash, often accompanied by hyperferritinemia. Macrophage activation syndrome (MAS) is observed in 15% of patients and is considered the most severe complication of the disease. Diagnostic methods and comprehensive data on the disease remain limited.
Objectives: This study aims to present demographic data, clinical features, lab values, management strategies, and outcomes of 93 patients with AOSD followed in a tertiary clinical center.
Methods: Data regarding the clinical features, treatment modalities, and survival outcomes were retrospectively collected from patient files that met Yamaguchi’s Criteria. Normally distributed continuous variables were reported as mean ± SD, while skewed variables were reported as medians with interquartile ranges (IQR ). Univariate analysis was conducted using descriptive statistics. Categorical variables were analyzed using the Chi-square test, and continuous variables were assessed using the t-test or Mann-Whitney U test as appropriate. Multivariate logistic regression was employed to identify independent predictors of disease progression, adjusting for confounders. Results were expressed as adjusted odds ratios with 95% confidence intervals, and a p-value < 0.05 was considered statistically significant.
Results: We included 93 patients with AOSD who were regularly followed up at our tertiary center, with ages ranging from 23 to 85 years and a mean age at onset of 33.60 ± 14.42 years. Among them, 64.5% (60/93) were female. Common clinical manifestations included fever (93.4%, 85/91), rash (65.6%, 59/90), arthritis (57.8%, 52/90), arthralgia (82.2%, 74/90), pharyngitis (%55.6, 50/90) and myalgia (%51.7, 46/89). Less frequent features were pleuritis (10.0%, 9/90), pericarditis (10.0%, 9/90), hepatomegaly (15.6%, 14/90), splenomegaly (23.3%, 21/90), and abdominal pain (17.0%, 15/88). Other symptoms included odynophagia in 40.7% of patients (33/81), hypertriglyceridemia in 32.8% (22/67), proteinuria in 22.7% (20/88), and lymphadenopathy (LAP) in 39.8% (35/88). Comorbid conditions were present in 77.6% of patients (59/76), while MAS was identified in 14.1% of cases (13/92). Malignancy was present in 3.9% of patients (3/76). The survival rate was 94.0% (79/84) at the time of follow-up. Patients who developed MAS and those who did not revealed significant age-related differences, as determined by an independent samples t-test. The mean age of MAS patients was 33.92 ± 10.72 years ( n = 12), while non-MAS patients had a mean age of 46.47 ± 14.19 years ( n = 79), (p=0.004). Similarly, the mean age of disease onset was significantly lower in MAS patients, averaging 27.67 ± 9.43 years ( n = 12), compared to 34.91 ± 15.27 years ( n = 74) in non-MAS patients, ( p =0.037). In the univariate analysis evaluating the relationship between age and MAS development, A negative association was observed between age and MAS occurrence, with a coefficient estimate of -0.09967 ( p = 0.0101), indicating that increasing age was significantly associated with a decreased risk of developing MAS. In the multivariate analysis assessing factors linked to MAS development, higher baseline ferritin levels were found to be a significant predictor. Elevated ferritin was positively associated with MAS occurrence ( p = 0.0489). Age showed a negative trend toward MAS development but did not reach statistical significance ( p = 0.0726). Additionally, proteinuria exhibited a borderline association with MAS ( p = 0.0888), and lower hemoglobin levels also demonstrated a non-significant trend ( p = 0.0949). Treatment approaches varied, with glucocorticoids being the most commonly used (93.3%, 84/90), followed by methotrexate (72.4%, 63/87), and anakinra (45.3%, 39/86). Biological agents such as tocilizumab (26.5%, 22/83) and canakinumab (15.5%, 13/84) were also employed. Additional treatments included hydroxychloroquine (HCQ) in 38.6% of patients (34/88), azathioprine (AZA) in 3.5% (3/86), cyclosporine A (CyA) in 3.5% (3/86), and Janus kinase inhibitors (JAKi) in 2.3% (2/86). The median highest glucocorticoid dose was 20.0 mg/day, with a lowest dose of 2.5 mg/day. 37.8% of patients (31/82) were able to completely stop using steroids.
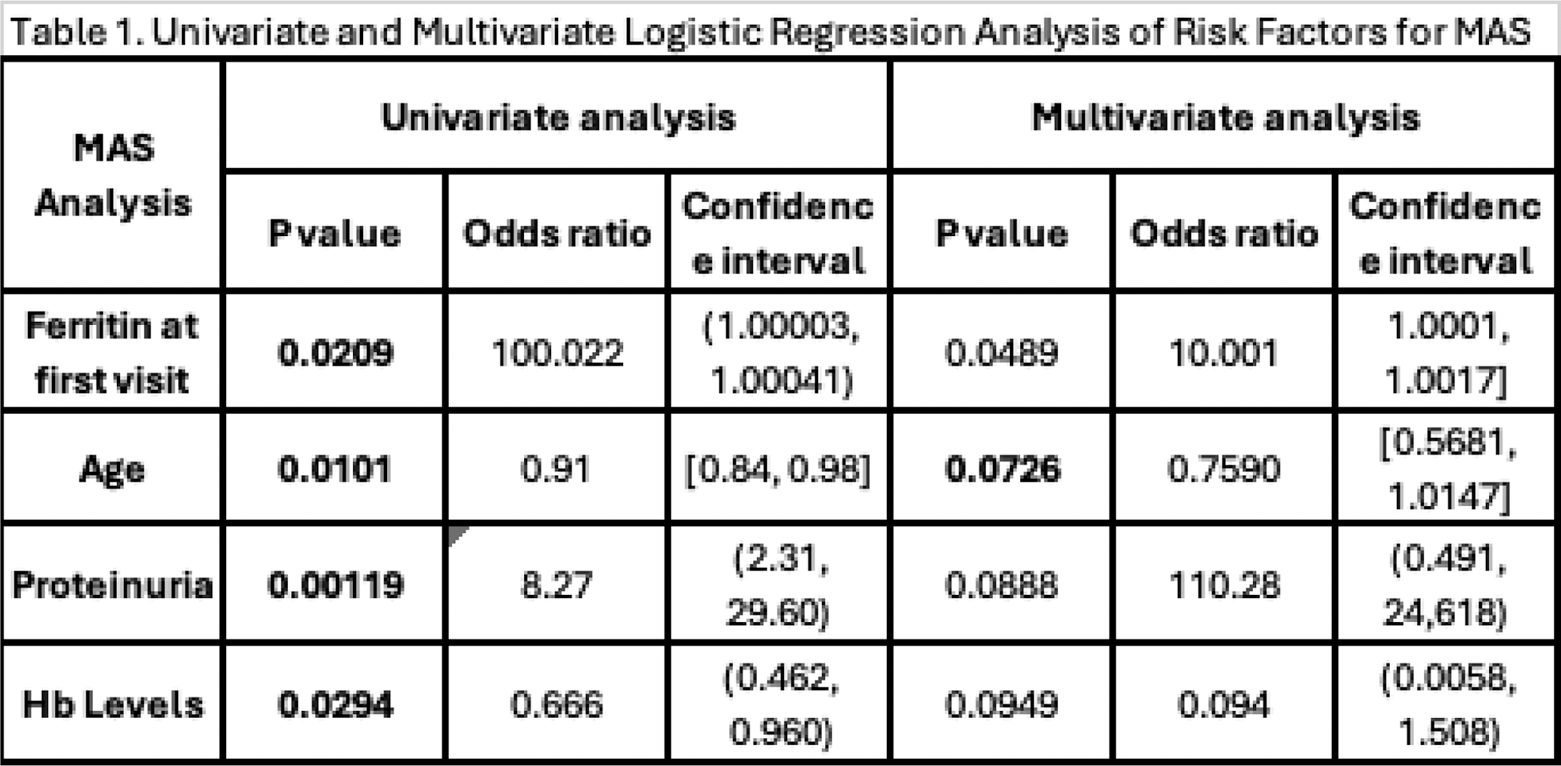
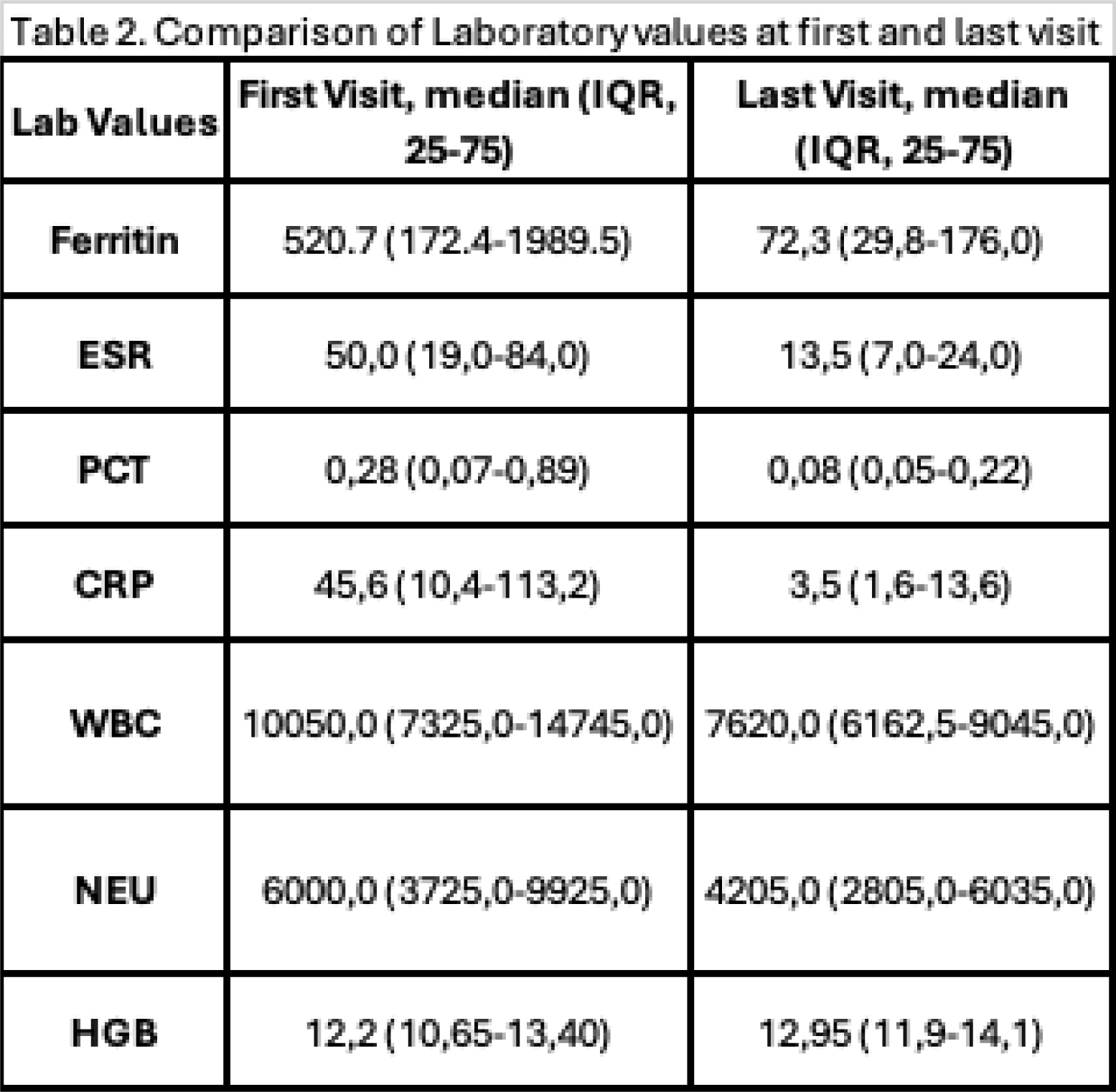
Conclusion: AOSD exhibits a wide range of clinical presentations and requires diverse treatment strategies. Younger age and earlier disease onset were significantly associated with an increased risk of MAS. Elevated baseline ferritin levels emerged as a significant predictor of MAS development in multivariate analysis. Although age, proteinuria, and hemoglobin levels showed trends toward association with MAS in the multivariate analysis, they did not achieve statistical significance. While glucocorticoids remained the primary treatment, the addition of immunosuppressive and biologic agents contributed to reducing and eventually stopping steroid use, with 37.8% of patients successfully discontinuing steroids. The cohort’s 94% survival rate and improved laboratory outcomes reflect the effectiveness of individualized treatment approaches. These findings highlight the importance of early identification of high-risk patients and the integration of targeted therapies to optimize disease management and enhance patient outcomes.
REFERENCES: NIL.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (