

Background: Gout is a metabolic disorder characterized by hyperuricemia, which often results in significant morbidity and disability. Its epidemiology shows marked variability across different regions in the United States, influenced by socioeconomic factors, healthcare access, and genetic predispositions. Chronic kidney disease (CKD), a prevalent comorbidity of gout, shares a bidirectional relationship with the condition. While CKD predisposes individuals to gout through impaired uric acid excretion, gout can worsen kidney function via hyperuricemia, chronic inflammation, and associated comorbidities. Despite these known associations, the temporal trends in the burden of gout and its interplay with CKD at a state level in the United States remain underexplored. This study aims to analyze three decades of data (1990–2021) on disability-adjusted life years (DALYs), incidence, prevalence, and mortality of gout across all 50 states, while examining their correlation with CKD epidemiology. Understanding these trends can guide targeted interventions to address the shared burden of these conditions.
Objectives: Gout exhibits varied epidemiological patterns across states in the United States, influencing disability-adjusted life years (DALYs), incidence rates, prevalence, and mortality. This study analyzes the percentage changes in DALYs, incidence, prevalence, death rates and its association with CKD incidence and prevalence across the United States from 1990 to 2021, utilizing data from all 50 states to examine trends in these health metrics over three decades.
Methods: The Global Burden of Disease database was used to extract age-standardized incidence, prevalence, death, and DALYs of gout from 1990 to 2021 for both males and females across U.S. states. The percent change in these rates between 1990 and 2021 was calculated.
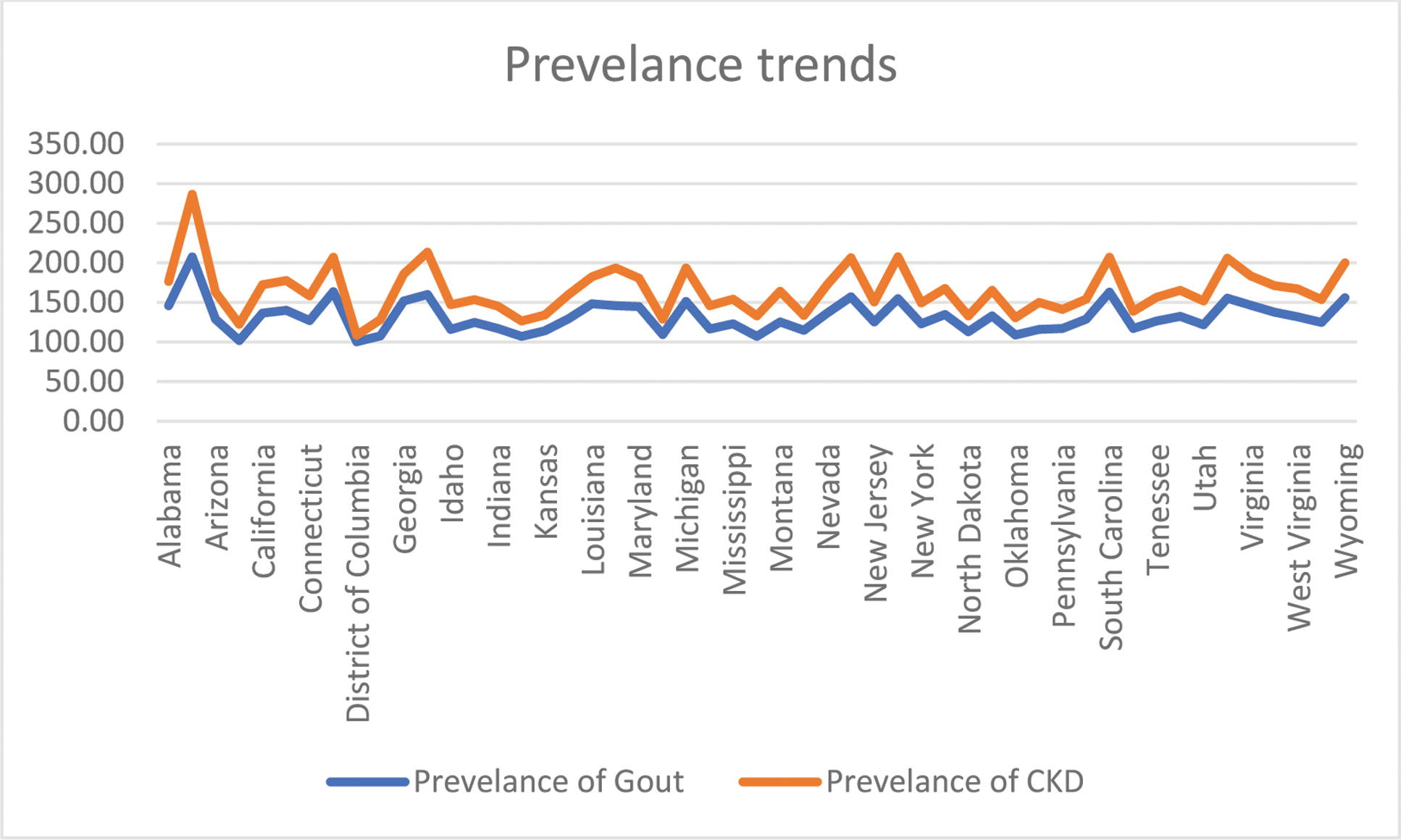
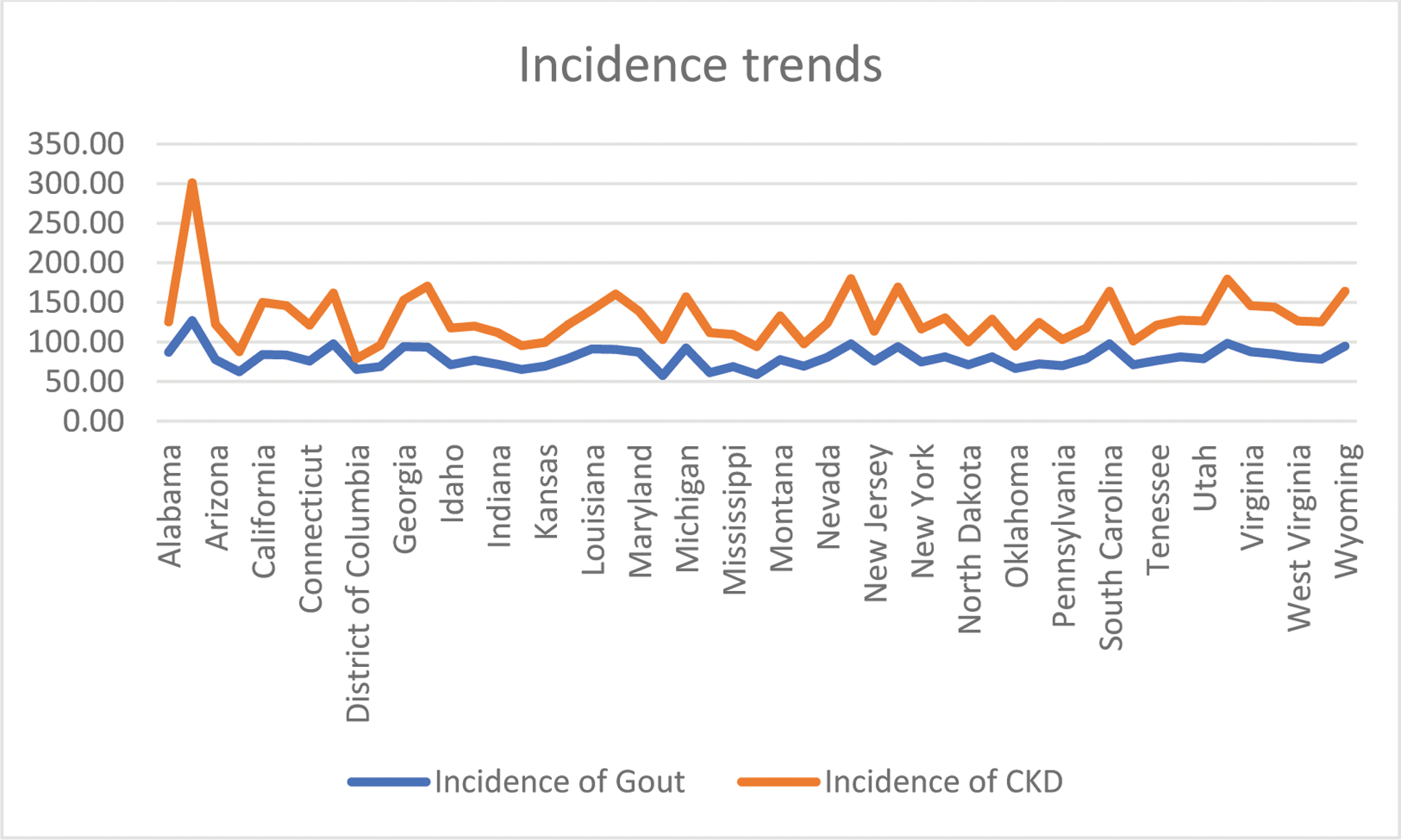
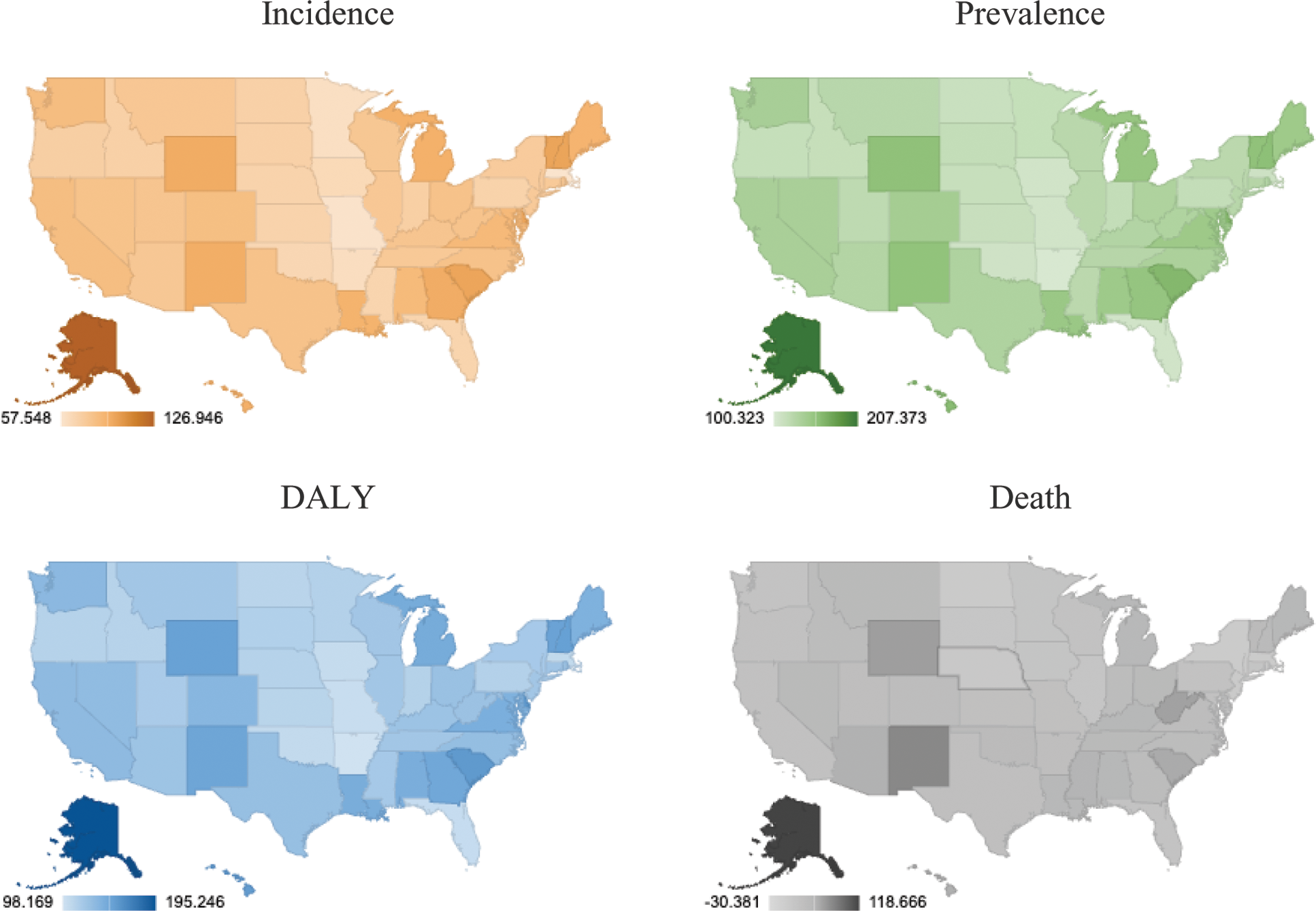
Results: Between 1990 and 2021, the incidence, prevalence, DALYs, and death rates related to gout inthe United States increased by 59.53%, 71.44%, 69.33%, and -0.49%, respectively. Disparities in disease burden were observed across states, with California and New York showing significant reductions in DALY rates, while Alaska and Mississippi faced higher rates. Prevalence and incidence also varied, with some regions showing progress and others experiencing persistent challenges. Death rates decreased in states like Hawaii and Colorado, while states such as West Virginia and Mississippi saw increases. Chronic kidney disease (CKD) and gout have a bidirectional association. CKD is an independent risk factor for gout, while gout may predispose to CKD through mechanisms like hyperuricemia, chronic inflammation, chronic NSAID use and co-morbid conditions such as hypertension and diabetes mellitus. The prevalence of gout is approximately 24% in individuals with reduced glomerular filtration rate (GFR) <60 ml/min/1.73 m², which is significantly higher compared to 2.9% among individuals with normal GFR. Gout prevalence increases two to threefold with each 30 ml/min/1.73 m² reduction in GFR. This association is strongest in those with severe renal impairment, where tophi presence correlates with lower creatinine clearance (≤30 ml/min). Our analysis of State-level data revealed similar variability in both gout and CKD incidence and prevalence. In the same time period as mentioned above, i.e. 1990-2021, the incidence and prevalence of CKD increased 45.75% and 29.05% respectively. This emphasizes the importance of addressing these conditions simultaneously in affected populations.
A comparison of prevalence trends in Gout and CKD across the country between 1991-2021.
A comparison of incidence trends in Gout and CKD across the country between 1991-2021.
Diagrammatic representation of percentage change in Incidence, Prevalence, Death and DALY across the country between 1991-2021.
Conclusion: Our findings highlight the complex relationship between kidney disease and Gout. Through our study we hope to drive further research into understanding this temporal association. Both these conditions are affected by similar multiplex of socio-economic factors, healthcare access, and public health policies that influence the increasing burden across different states. Modifiable risk factors such as alcohol intake, along with unmodifiable factors like genetic association, prevalent cardiovascular disease and environmental factors (e.g., colder climates), contribute to regional differences in disease patterns. Addressing these disparities through targeted interventions is essential for improving population health and reducing the burden of gout and CKD across the United States.
REFERENCES: [1] Stamp LK, Farquhar H, Pisaniello HL, Vargas-Santos AB, Fisher M, Mount DB, Choi HK, Terkeltaub R, Hill CL, Gaffo AL. Management of gout in chronic kidney disease: a G-CAN Consensus Statement on the research priorities. Nat Rev Rheumatol. 2021 Oct;17(10):633-641. doi: 10.1038/s41584-021-00657-4. Epub 2021 Jul 30. PMID: 34331037; PMCID: PMC8458096.
[2] Kannuthurai V, Gaffo A. Management of Patients with Gout and Kidney Disease: A Review of Available Therapies and Common Missteps. Kidney360. 2023 Sep 1;4(9):e1332-e1340. doi: 10.34067/KID.0000000000000221. PMID: 37526648; PMCID: PMC10550007.
[3] Vargas-Santos AB, Neogi T. Management of Gout and Hyperuricemia in CKD. Am J Kidney Dis. 2017 Sep;70(3):422-439. doi: 10.1053/j.ajkd.2017.01.055. Epub 2017 Apr 26. PMID: 28456346; PMCID: PMC5572666.
Acknowledgements: NIL.
Disclosure of Interests: None declared.
© The Authors 2025. This abstract is an open access article published in Annals of Rheumatic Diseases under the CC BY-NC-ND license (